This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Although H. pylori infection is often associated with gastric manifestations, increasing evidence is drawing attention to its role in extragastric diseases. Some studies show an association between H.pylori infection and dermatological and autoimmune diseases.
1. Dermatological and autoimmune diseases
Several studies suggest an association and possible causality of H. pylori infection in some dermatological diseases. Among them, rosacea and some immune diseases such as idiopathic thrombocytopenic purpura, psoriasis, alopecia areata, and urticaria are the most studied diseases. However, the evidence clearly shows that a significant association with H. pylori infection occurs only in some of these diseases, many of which have yielded conflicting results, which requires must be further investigated with more appropriate statistical design and methodologies. As for autoimmune diseases, they are characterized by dysregulation of the immune system, leading to a loss of tolerance to autoantigens. These diseases are believed to have a multivariable etiology and infectious agents can cause them. The immune response against H. pylori can induce inflammation potentially leading to the development of cross-reactive antibodies. Rosacea is a chronic disease with skin manifestations such as facial erythema, edema, papules, vesicles and pustules usually located in the center of the face.
H. pylori infection and rosacea
A risk association has been observed between H. pylori infection and rosacea, and treatment of this bacterial infection significantly reduces the severity of that dermatological disorder . Other authors observed similar results and began recommending that patients with H. pylori-positive rosacea be treated with eradication. However, a meta-analysis concluded that the cause-effect relationship was weak between this disease and H. pylori infection (OR = 1.68, 95% CI: 1.100-2.84, P = 0.052) ) and H. pylori eradication therapy did not achieve the statistical significance required for a series recommendation, (RR = 1.28, 95% CI: 0.98 -1.67, P = 0.069). The contrast of results found in the literature may be related, among other things, to large differences in the statistical and methodological designs used.

H. pylori infection and psoriasis
Psoriasis is a chronic, non-communicable, genetic and autoimmune skin disease affecting the skin and joints. Its association with H. pylori infection has been studied with the search for antibodies against H. pylori in psoriasis patients without known gastrointestinal complaints. Recently, a meta-analysis found strong evidence for this association (OR = 1.19, 95% CI: 1.15-2.52, P = 0.008) and emphasized that the ratio H. pylori infection was, interestingly, significantly higher in patients with moderate levels. and severe psoriasis (OR = 2.27; 95% CI: 1.42-3.63, I 2 = 27%) but not in patients with milder disease (OR = 1.10; CI 95%: 0.79-1.54, I2 = 0%). Another disease commonly associated with H. pylori infection is chronic urticaria, a clinical condition presenting with itchy, erythematous, or swollen urticaria. Studies show conflicting evidence about a cause-and-effect link of H. pylori with chronic urticaria. Interestingly, a meta-analysis showed that improvement of chronic urticaria was not directly related to H. pylori eradication, but to antibiotic therapy used, and even to treatment. Ineffective treatment, significant remission of chronic urticaria was observed in these patients.
H. pylori infection and alopecia areata
Alopecia areata (AA), an autoimmune disease, leads to hair loss and may present differently in affected individuals. There are few published studies on the association of AA with H. pylori infection. In a case-control study in Iran, a statistically significant risk association was observed (OR = 2,263, 95% CI: 1,199-4.273); however, limitations of the study such as the inability to control for some confounding variables undermined this evidence.
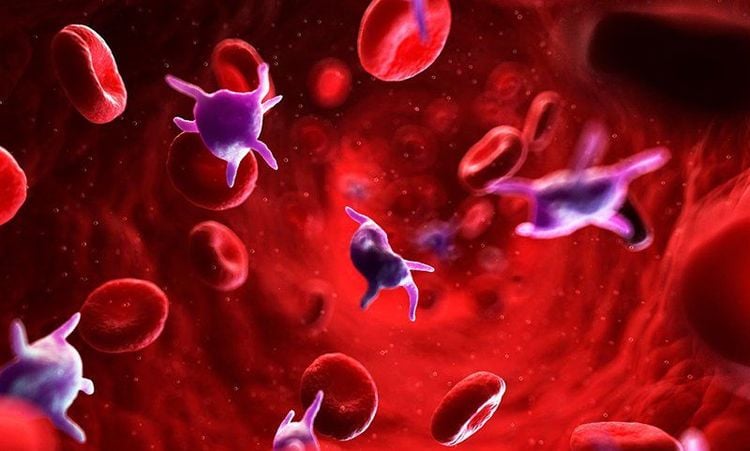
H. pylori infection and idiopathic thrombocytopenic purpura
Idiopathic thrombocytopenic purpura (ITP) is a condition that results from an individual's platelet destruction mediated by antiplatelet antibodies . Several studies link the relationship between H. pylori infection and ITP. Although the pathogenesis involved in this process is inconclusive, some authors suggest that CagA stimulates the synthesis of anti-CagA antibodies that cross-react with ITP-induced platelet surface antigens. The first correlation of this pathogenicity was observed with an increase in the patient's platelet count after eradication of H. pylori. Other studies have also been performed to evaluate remission of PTI after treatment of H. pylori infection.
clinical management guidelines
2. Conclusion
Further studies are needed to assess whether bacterial eradication could be a suitable alternative treatment for a large number of health problems. Finally, the beneficial association of H. pylori infection with some extragastric diseases needs to be studied in the future to evaluate the use of the bacteria and its products in new treatment and prevention regimens. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References Santos MLC, de Brito BB, da Silva FAF, Sampaio MM, Marques HS, Oliveira e Silva N, de Magalhães Queiroz DM, de Melo FF. Helicobacter pylori infection: Beyond gastric manifestations. World J Gastroenterol 2020; 26(28): 4076-4093 [PMID: 32821071 DOI: 10.3748/wjg.v26.i28.4076]