This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Dietary and lifestyle modifications are effective interventions for GERD, despite the fact that there are few robust published data. According to the treatment used at a UK county general hospital, dietary and behavioral modifications have also been found to be very effective in managing laryngopharyngeal reflux.
1. Lifestyle changes in the treatment of laryngeal reflux
Recommended methods to treat laryngopharyngeal reflux :
Treat obesity / overweight
Reduce daily calorie intake Aerobic physical activity Change eating habits:
Increase fiber intake Increase intake of fruits and vegetables Reduce intake of spicy and sweet foods Reduce intake of carbohydrate drinks Reduce alcohol and coffee intake Elevate the head of the bed
Avoid strenuous exercise

Methods that are unlikely to improve the condition:
Lose weight at a normal BMI Reduce the amount of acidic drinks (orange or apple juice) Reduce the amount of tomatoes, ketchup, mint and garlic Reduce quantity of tomatoes, ketchup, mint and garlic Reduce smoking
2. Eating habits
Although there are few data on this, in clinical practice different foods are indicated to influence the occurrence of reflux and in general, patients are advised not to take them. late evening food.
High-fat foods and chocolate are indicated empirically as foods that can reduce lower esophageal sphincter pressure or prolong gastric emptying time; however, there are no discontinuation trials evaluating the impact on gastroesophageal reflux disease outcomes. Heartburn can be aggravated by spicy foods by directly irritating the already inflamed esophageal lining. In particular, Nebel et al. described that 88% of patients cited spicy foods as the cause of their heartburn. Orange juice was associated with GERD symptoms even when orange juice infusion did not change lower esophageal sphincter pressure.
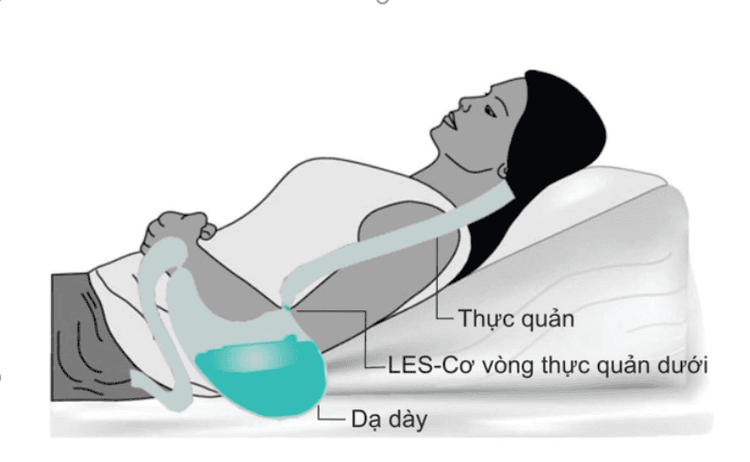
3. Sleeping position
There are various indications that the body position during sleep is related to the reflux of gastric juice into the esophagus. Sleep duration alters the underlying physiological mechanisms that provide physiological protection against GERD. Mechanisms of sleep depression include heartburn warning signals, frequency of swallowing, and inhibition of salivation. Several studies have shown that esophageal acid clearance is significantly prolonged during sleep compared to the waking state; this holds true even when the sleeping subject is compared with the awake subject in the supine position.
Headboard height can be achieved by placing 15–20cm blocks under the foot of the bed at the headboard or a foam pad under the mattress. Randomized trials have shown that this practice can reduce exposure to esophageal acid and lead to shorter reflux times and more rapid clearance of the esophagus. Elevating the head of the bed is important for people with nocturia or laryngeal symptoms. The right-side lying position has also been shown to cause prolonged reflux time and increased relaxation of the lower esophageal sphincter, so patients with gastroesophageal reflux disease or laryngeal reflux should avoid lying on their side. like this
4. Exercise
Exercise has been shown to be a protective factor against reflux. In particular, in a large population-based study, a correlation was noted between the number of exercise sessions lasting at least 30 minutes and a reduced risk of GERD symptoms (OR 0). ,5; 95% CI 0.4–0.7) .
Usually, scheduled body weight loss programs, which are considered helpful for reducing reflux symptoms, are often associated with physical activity. Indeed, a mechanism of exercise-enhanced antireflux barrier, possibly mediated by striated muscle, has been hypothesized. Furthermore, Nocon and colleagues also reported that subjects with GERD symptoms performed worse physically than those without symptoms. However, esophageal acid exposure was significantly increased in healthy volunteers and GERD patients during intense exercise compared with no exercise. Pandolfino et al. have suggested that anatomical injury of the oesophageal junction, as a consequence of frequent exercise-related abdominal distension, may predispose to exercise-induced reflux. Various studies have suggested that an autonomous physical activity may play a role in the induction of GERD symptoms (ie, running, cycling, exercise). It has been suggested that gastroesophageal reflux disease may be increased in athletes because of reduced gastrointestinal blood flow, altered hormone secretion, and altered motor function of the esophagus and heart. ventricles, and restricted body positions during exercise.
5. Conclusion
The management of laryngeal reflux can be divided into lifestyle modification, medical treatment and/or surgery. Behavioral changes and lifestyle modifications are considered first-line treatments with the lowest chance of side effects. Weight loss, smoking cessation, alcohol avoidance, changes in eating habits, and elevation of the head during sleep should be recommended for the patient. As for medical therapy, currently, treatment is focused on increasing the pH of the reflux substance, so it is advisable to start with PPIs twice daily for a period of 8-12 weeks. Tolerant patients with objective evidence (reflux monitoring) of ongoing reflux as the cause of symptoms should be considered for alternative therapies, such as visceral pain modifiers or endoscopic anti-reflux surgery.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesIrene Martinucci, Nicola de Bortoli, Optimal treatment of laryngopharyngeal reflux disease, Ther Adv Chronic Dis. 2013 Nov; 4(6): 287–301. Altman K., Prufer N., Vaezi M. (2011) A review of clinical practice guidelines for reflux disease: towards creating a clinical protocol for the otolaryngologist. Laryngoscope 121: 717–723 [PubMed] [Google Scholar] Anderson J., Jhaveri M. (2010) Reductions in medications with significant weight loss with behavioral intervention. Curr Clin Pharmacol 5: 232–238 [PubMed] [Google Scholar] Bardhan K., Strugala V., Dettmar P. (2012) Reflux revisited: advancing the role of pepsin. Int J Otolaryngol 2012: 646901. [PMC free article] [PubMed] [Google Scholar] Bough I., Jr, Sataloff R., Castell D., Hills J., Gideon R., Spiegel J. (1995) Gastroesophageal reflux laryngitis resistant to omeprazole therapy. J Voice 9: 205–211 [PubMed]














