This is an automatically translated article.
The article was consulted professionally with BS. Nguyen Hai Ha - Head of Vaccine Unit - Pediatric Outpatient Department - Pediatric Center - Vinmec Times City International Hospital.Japanese encephalitis is a common infectious disease in the Asia-Pacific region, with no specific treatment, with an incidence of 67,900 cases/year (incidence rate: 1.8/100,000 population), mortality rate is 25-30%, 50% of patients live with severe neurological sequelae. Therefore, information about Japanese encephalitis is still one of the issues that need attention to protect everyone's health.
1. Features of Japanese encephalitis
Japanese encephalitis is an acute, blood-borne infectious disease that infects the central nervous system in adults and children caused by Japanese encephalitis virus of the Togaviridae family, genus Flavivirus. Japanese encephalitis virus is a heat-resistant virus, inactivated at 56 degrees Celsius for 30 minutes and 2 minutes at 100 degrees Celsius. The virus can survive for up to several years in a frozen state. .Sources of Japanese encephalitis are mainly wild birds and livestock such as pigs, buffaloes, cows, horses.
Transmission route: is transmitted by the Culex mosquito. Mosquitoes will be infected with the Japanese encephalitis virus after sucking blood from infected animals, and then transmitted to humans through mosquito bites. Culex mosquitoes breed strongly in the summer, so Japanese Encephalitis often breaks out in the summer, especially from May to July.
2. Incubation period of Japanese Encephalitis
2.1. Typical body
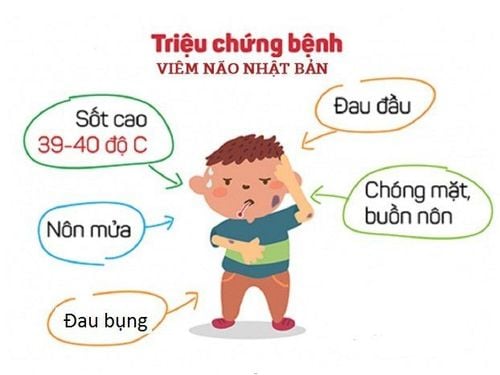
Onset period:
This period of the disease corresponds to the time when the virus crosses the blood-brain barrier and causes cerebral edema, causing the manifestations of meningococcal syndrome. The onset of the disease is very sudden with a high fever of 39 - 40°C or more. Patients may experience headache, abdominal pain, nausea, and vomiting. In the first 1-2 days of the disease may appear stiff neck, increased muscle tone, eye movement disorders, confusion or loss of consciousness, increased tendon reflexes. In some young children, loose stools, abdominal pain, and vomiting may appear like bacterial infection - food poisoning. The full-blown period:
From the 3rd - 4th day to the 6th - 7th day of the disease: The virus invades the brain parenchyma and destroys nerve cells, the prominent symptom in the full-blown phase is the appearance of signs of brain damage and focal neurological damage. On the 3rd - 4th day of the disease, the symptoms of the onset period do not decrease but increase. Patients from excited delirium, consciousness disturbance, gradually go into a deep coma. Symptoms of autonomic disorders also increase: Profuse sweating, red, pale skin, breathing disturbances and increased secretions in the bronchial tubes, pulse is often fast, weak, and blood pressure increases. Patients with delirium, hallucinations, agitation, increased muscle tone cause the patient to lie in convulsions and have episodes of torsion, rigidity or tremor of the facial and limb muscles. Some patients appear fixed state, keep the posture. Local symptoms: Paralysis of legs and arms; The cranial nerves are damaged, especially the ophthalmic and facial nerves (VII). Patients usually die within the first 7 days, patients who pass this period have a better prognosis.

White blood cells usually increase by 15,000-20,000/mm3, mainly neutrophils increase to 75 - 85%, erythrocyte sedimentation rate increases. Aspiration and testing of cerebrospinal fluid: CSF pressure is increased, clear fluid, protein is slightly increased (60 - 70 mg%), cells are slightly increased (less than 100 cells/mm3), at first neutrophils make up dominated, later on, lymphocytes prevailed. Glucose in the cerebrospinal fluid was little changed or increased slightly. Ophthalmoscopy in the acute phase often reveals papilledema, sometimes with edema and hemorrhage. Remission period
The main manifestation is complications and sequelae. Usually, by the 2nd week, the disease gradually improves, the temperature drops and no fever is gone by about 10 days if there is no superinfection. Along with the decrease in temperature, encephalopathy - meningoencephalopathy syndrome also gradually disappeared. While the toxic infection syndrome and the encephalo-meningeal syndrome subsided, the focal neurological lesions were more prominent than before. There may be psychiatric sequelae, focal neurological signs such as paralysis of limbs, cranial nerves.
2.2. Atypical bodies
Hidden form: It is found that after epidemics, the number of people who do not have the disease but still have an immune response accounts for a very high rate (hundreds of times the number of infected people). Specific body: Only toxic infection syndrome (high fever, congestion, headache), no symptoms of encephalopathy syndrome. Meningitis form: Found in older children and young adults, Thus, during the incubation period of Japanese encephalitis, there are no symptoms of the disease. Currently, there is no specific treatment for Japanese encephalitis, so vaccination against the disease and killing mosquitoes around the environment is the most effective way to prevent Japanese encephalitis.Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














