This is an automatically translated article.
Intracerebral hemorrhage is bleeding from a blood vessel in the brain parenchyma. It is usually caused by high blood pressure. Typical symptoms are sudden onset of headache, nausea, focal deficits in neurologic function, and impaired consciousness. Treatment includes hypertension control, supportive therapy, and surgical removal of the hematoma.
1. What is bleeding in the brain?
Intracerebral hemorrhage is bleeding from a blood vessel in the brain parenchyma. Bleeding in the brain is usually caused by high blood pressure. Typical symptoms of intracerebral bleeding include often sudden onset of headache, nausea, focal deficits in neurologic function, and impaired consciousness.
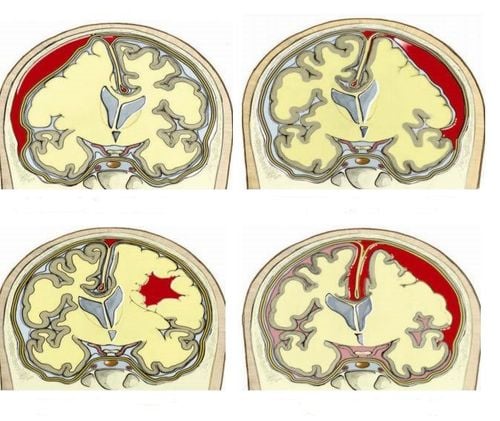
Blood from a bleeding site in the brain will accumulate in a mass and may spread around pressing on adjacent brain tissue, causing neurological dysfunction. Large hematomas increase intracranial pressure. Pressure from the supratental hematoma and accompanying cerebral edema can cause transtentorial herniation, compressing the brain stem and often causing secondary bleeding in the midbrain and pons. If the hematoma ruptures into the ventricular system, also known as intraventricular hemorrhage, the blood can cause acute hydrocephalus. Hematomas at the cerebellum site can spread and block the 4th ventricle, as well as lead to acute hydrocephalus or blood that can penetrate the brain stem. Hematomas > 3 cm in diameter in the cerebellum may cause midline shift or brain herniation.
Conditions such as pons or midbrain bleeding, intraventricular bleeding, brain herniation, acute hydrocephalus or blood dissection into the brain stem can be dangerous for the patient and lead to impaired consciousness, coma and even death.
2. Causes of bleeding in the brain
Causes of bleeding in the brain as a result of atherosclerosis leading to a ruptured small artery, mainly due to chronic arterial hypertension. Such intracerebral bleeding is often large, single, and has severe consequences. Other risk factors that may increase the risk of bleeding in the brain due to atherosclerosis include
Smoking Obesity High-risk diet: high in saturated fat, trans fat into energy Cocaine use Sometimes other sympathomimetic drugs can cause transient severe hypertension and lead to bleeding in the brain. Less common causes of bleeding in the brain such as
Congenital aneurysm Arteriovenous malformation or other vascular malformation Mushroom aneurysm Cerebral infarction Primary or metastatic brain tumor Anticoagulation overdose Any normal blood cells Intracranial artery separation Moyamoya disease Vasculitis Hemorrhagic pathology.

Hút thuốc lá là yếu tố có thể làm tăng nguy cơ chảy máu trong não
3. How dangerous is bleeding in the brain?
Bleeding in the brain can cause symptoms including:
Headache: typically begins with a sudden headache, often during activity. However, in the elderly, headaches may be mild or dizzy. Loss of consciousness: usually occurs within seconds or minutes. Nausea, vomiting Delirium Partial or generalized convulsions are also common. Neurologic deficits are often sudden and progressive. If the brain bleeds in the hemisphere, it can cause hemiplegia. Posterior fossa location results in impaired neurologic function of the brainstem or cerebellum (eg, skewed eyes or ophthalmoplegia, constricted pupils, snoring, or coma).
In addition, large intracerebral bleeding can lead to death within a few days in about half of patients. In patients who were able to overcome the intracerebral hemorrhage, consciousness and neurological deficits gradually recovered to varying degrees as the hematoma was slowly absorbed. Some other patients had a better outcome, with only a few mild neurological deficits because bleeding caused less brain tissue damage than infarction.
4. Diagnosis of bleeding in the brain
The diagnosis of intracerebral hemorrhage is suggested by the sudden onset of symptoms such as headache, focal deficits in neurologic function, and impaired consciousness, particularly in patients with risk factors. Diagnostic methods for bleeding in the brain are CT or MRI scans. Neuroimaging is usually diagnostic. If neuroimaging does not show bleeding but subarachnoid hemorrhage is clinically suspected, a lumbar puncture is necessary. CT angiography, performed within a few hours of the onset of bleeding, may show contrast media extravasation into the hematoma, also known as the dot sign, which indicates bleeding The brain is still ongoing and suggests a more extensive hematoma, and the patient's prognosis is often poor.
Bleeding in the brain needs to be differentiated from diseases such as:
Ischemic stroke Subarachnoid hemorrhage Other causes of acute neurological deficit eg seizures, hypoglycemia. Therefore, it is necessary to conduct blood glucose measurement at the bed.

Đau đầu đột ngột là triệu chứng chảy máu trong não
5. Treatment of bleeding in the brain
Treatments for intracerebral bleeding include control of hypertension, supportive therapy for some patients, and surgical removal of the hematoma. Surgical removal of the hematoma should be performed for hematomas > 3 cm.
Contraindications to the use of anticoagulants and antiplatelet agents in patients with cerebral bleeding. If the patient has ever used anticoagulants, fresh frozen plasma, prothrombin complex concentrate, vitamin K or platelet transfusion may be indicated. Dialysis can remove about 60% of dabigatran.
According to the 2015 recommendations of the American Stroke Association and the American Heart Association, hypertension can be reduced to a safe level with a systolic blood pressure of 140 mmHg in people with a systolic blood pressure of 150 mmHg to 220 mmHg and in the absence of contraindications to emergency hypotension. If systolic blood pressure is > 220 mmHg, hypertension may need to be treated aggressively with continuous intravenous infusion. In such cases, systolic blood pressure must be continuously and more frequently monitored. Intravenous nicardipine at an initial dose of 2.5 mg/h, titrated in increments of 2.5 mg/hr every 5 minutes to a maximum of 15 mg/hr as needed to reduce systolic blood pressure by 10 to 15%.
A hematoma with a radius > 1.5 cm in the cerebellar hemisphere can cause midline shift or brain herniation, so surgical removal of the hematoma is often a life-saving method. Early surgical removal of a large hematoma in the lobe of the brain can also be life-saving, but it is often complicated by recurrent bleeding, sometimes aggravating neurological deficits. Surgery to remove a hematoma deep inside the brain is rarely indicated because of the high mortality rate of surgery and the complication of neurologic deficits that are often severe. Anticonvulsants are not usually used in prophylactic regimens; they are used only when the patient has a seizure.
In short, intracerebral hemorrhage is a condition in which blood flows from a blood vessel in the brain parenchyma. It is usually caused by high blood pressure. Typical symptoms are abrupt onset of headache, nausea, focal deficits in neurological function, and impaired consciousness. Bleeding in the brain can cause dangerous conditions and can even lead to death. Therefore, when there are abnormal manifestations, it is necessary to call an ambulance to receive help from medical staff.
Vinmec International General Hospital is the address for examination, treatment and prevention of diseases, including Neurology. When performing the examination process at Vinmec, customers will be welcomed and used modern facilities and equipment along with perfect medical services under the guidance and advice of experts. Good doctors, well-trained both at home and abroad.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.