This is an automatically translated article.
The article is written by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Inflammatory diarrhea is a common feature of gastrointestinal histoplasmosis and inflammatory bowel disease. Similarities in presentation, gastrointestinal (GI) involvement, and inflammation are the reasons why histoplasmosis resembles inflammatory bowel disease. However, it is not considered as one of the differential diagnoses in these diseases.
1. Overview
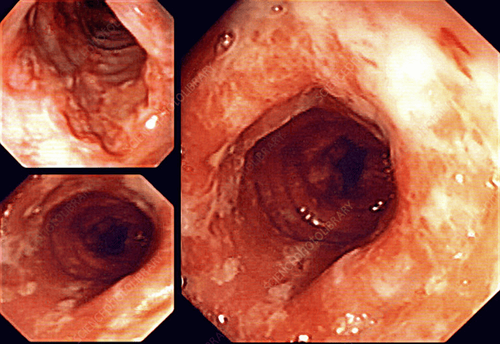
Histoplasma capsulatum (H. capsulatum) var. capsulatum is a dimorphic fungus that is widespread around the world. In the United States, histoplasma fungi are mainly endemic to the Ohio and Mississippi valleys. In the environment, it exists in the form of mycelium, which produces spores that humans inhale, which begin to infect. In the body, the spores switch to the yeast stage, evade interstitial destruction, and are transported by macrophages to any organ in the body. This leads to disseminated histoplasmosis (DH). Gastrointestinal (GI) spread, known as gastrointestinal histoplasmosis, most commonly involves the colon and terminal ileum.
2. Symptoms of gastrointestinal histoplasmosis
The most common symptoms in patients with gastrointestinal histoplasmosis are abdominal pain and inflammatory diarrhea. Inflammatory bowel disease (IBD) is characterized by chronic inflammation of the intestinal mucosa through a complex immune-mediated mechanism. The two main subtypes of inflammatory bowel disease, Crohn's disease and ulcerative colitis (UC), are based on histological involvement of the intestine. Common symptoms of inflammatory bowel disease include:
Diarrhea or constipation Hemophilia Severe diffuse abdominal pain Unintentional weight loss Apatite is greatly reduced, Fatigue and fever. Inflammatory diarrhea is a common feature seen in both gastrointestinal histoplasmosis and inflammatory bowel disease. Similarities in presentation, related patterns of the gastrointestinal (GI) tract, and inflammation are the reasons gastrointestinal histoplasmosis is similar to inflammatory bowel disease. However, it is not considered as one of the differential diagnoses in these patients. In patients with diagnosed inflammatory bowel disease, gastrointestinal histoplasmosis may be confused with an exacerbation of the underlying disease.
3. Diarrhea in inflammatory bowel disease
Inflammatory bowel disease is a disease characterized by chronic inflammation of the intestinal mucosa through a complex immune-mediated mechanism. The exact cause of inflammatory bowel disease is unknown, but it is thought to be due to an abnormal immune response of the intestinal mucosa to environmental agents, leading to inflammation of the gastrointestinal mucosal epithelium. . The immune system of the gastrointestinal tract plays an important role in providing an appropriate immune response to harmful pathogens, while conferring an immune tolerance to harmless food materials. and similar flora. The literature reports an increase in the incidence and prevalence of inflammatory bowel disease in adults and children. Although the exact reason for this increase is unclear, it is believed that changes in lifestyle and nutritional habits may play an important role.
The Rochester Epidemiology Project noted an increase in the incidence and prevalence of inflammatory bowel disease between 2001 and 2011, but this is attributed to an increase in overall life expectancy. Against the backdrop of increasing westernization and industrialization, Asian countries such as India, China and Iran are reporting a significant increase in the number of inflammatory bowel diseases
4. Classification of inflammatory bowel disease
Inflammatory bowel disease can be classified into 2 main subtypes based on the clinical presentation and distinct pathological features. Specific:
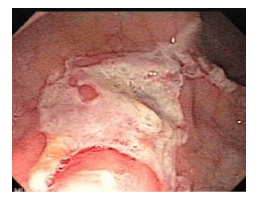
Ulcerative Colitis Ulcerative colitis is a chronic inflammatory condition characterized by recurrent and remission episodes of inflammation that are limited to the lining of the colon. The mucosa is involved in a continuum with almost all reported cases of rectal involvement.
Crohn's disease Crohn's disease is a chronic inflammatory condition characterized by total (transmural) adhesions of the intestine and the presence of "jumping" lesions (diseased areas of the midgut that appear normal). ). It usually involves the ileum and proximal part of the colon. However, any part of the gastrointestinal tract may be involved. Symptoms in patients with IBD depend on the severity of the inflammation and can range from very mild to severe. Common symptoms of IBD include diarrhea or constipation, hemophilia, severe diffuse abdominal pain, unintentional weight loss, markedly reduced appetite, fatigue, and fever.
5. Evaluation of patients with inflammatory bowel disease
The first step in evaluating a patient with inflammatory bowel disease includes a detailed history and physical examination. History can be important in differentiating patients with inflammatory bowel disease from other functional and functional causes. A thorough physical examination in a patient with inflammatory bowel disease may reveal mild to moderate abdominal pain without distention.
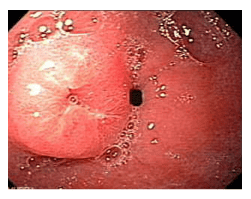
Initial laboratory tests may show elevation of inflammatory markers, i.e. ESR and CRP. In symptomatic patients presenting with acute diarrhea, stool studies to rule out infectious causes such as C. diff and parasites should also be performed. Fecal calprotectin, a fecal marker for inflammation, can also be used to determine the presence of enteritis in clinically suspected patients. If fecal calprotectin values are above the reference range (50 mcg/g), ileocoloscopy (ileocoloscopy) with biopsy and/or small bowel imaging may be used for diagnosis. inflammatory bowel disease and assessment of mucosal inflammation.
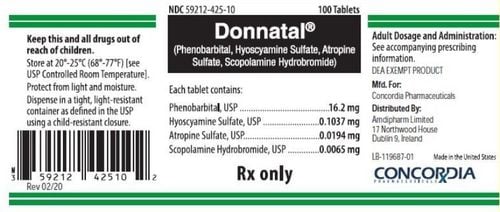
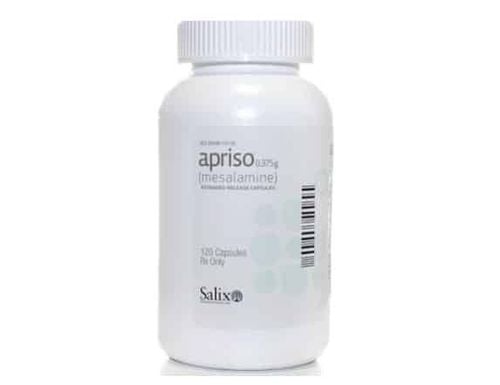
Although endoscopic ileostomy with biopsy is the method for definitive diagnosis and assessment of inflammation, imaging modalities such as X-ray, computed tomography (CT) bowel, resonance from the intestines (preferred over CT of the intestine), capsule endoscopy or endoscopic ultrasonography of the GI tract may also be used in certain situations. The management of inflammatory bowel disease is primarily focused on symptom relief, rapid onset of remission without steroids, prevention of disease complications, and its treatment. The choice of therapy is based on the severity of the disease, its response to previous therapy, and the characteristics of the individual patient. Some agents used in the treatment of inflammatory bowel disease include Sulfasalazine, Mesalamine, Olsalazine, Balsalazide, Corticosteroids, Azathioprine, 6-Mercaptopurine, Methotrexate, Infliximab, Adalimumab, and Tacrolimus. Because of the chronic inflammation in inflammatory bowel disease, patients can have a variety of complications. These complications are often associated with a specific subtype of inflammatory bowel disease, but some may be shared between the two. Complications include:
Common complications: Colon cancer, arthritis, uveitis, primary sclerosing cholangitis, and hypercoagulable states. Ulcerative colitis: Megacolon toxicity, colon perforation and severe dehydration. Crohn's disease: Intestinal obstruction, ulcers, fistulas, and anal fissures.
6. Conclusion
H. capsulatum is a dimorphic fungus endemic to the Ohio and Mississippi valleys. H. capsulatum var. capsulatum. H. capsulatum exists as a mycelium in the environment and inhalation of the spores produced by this form can infect humans. After infecting the host, it transforms into the pathogenic yeast form, which multiplies inside macrophages and avoids intracellular killing. Macrophages can disseminate the fungus to any organ in the body, leading to histoplasmosis. In the gastrointestinal tract, the most common sites of involvement are the terminal ileum and colon because of the abundance of lymphatic tissue.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Dahiya D, Kichloo A, Singh J, Albosta M, Wani F. Histoplasmosis and inflammatory bowel disease: A case report. World J Gastrointest Endosc 2021; 13(1): 24-32 [PMID: 33520104 DOI: 10.4253/wjge.v13.i1.24]