This is an automatically translated article.
Article written by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Celiac is a chronic autoimmune disease caused by a reaction to gluten in food. The disease has a genetic factor and in clinical practice, manifestations are quite diverse from no symptoms to faint symptoms or severe cases can have typical malabsorption symptoms such as chronic diarrhea, anemia, etc. iron deficiency blood, thin weight loss...
This is considered a rare digestive disorder in which it is common in children, however, in recent years, the detection rate of this disease has increased along with the recording of many clinical symptoms outside the gastrointestinal tract. and seen in many age groups.
1. What causes Celiac disease?
Guten plays an important role in the pathogenesis of Celiac. Gluten is the prolamin (plant protein) in grains including giadin in wheat, Sealin in rye, hordein in barley. These are peptide chains rich in proline and glutamine and are therefore difficult to be broken down by gastric acid, pancreatic enzymes or intestinal enzymes, even in healthy individuals.
In normal humans, the epithelial layer of the intestinal mucosa does not allow passage of the wheat-derived gliadio peptide chains. Celiac is a chronic autoimmune disease caused by exposure to gluten in the lining of the digestive tract.
In this disease, the physiological protective barrier of intestinal epithelial cells is disrupted by giadin chains passing through the epithelial layer, activating a variety of immune mechanisms that damage intestinal epithelial cells. .
2. What is histopathological diagnosis?
Histopathology (English: Histopathology, compound of three Greek words: ἱστός histos "tissue", pathos πάθος "suffering", and -λογία -logia "study") refers to the use of the microscope tissue examination to study the manifestations of the disease.
Specifically, in clinical medicine, histopathology refers to the examination of a biopsy or surgical specimen by a pathologist, after the specimen has been processed and histological sections are placed on glass slides. In contrast, cytology examines free cells or tissue microscopic fragments (as "cell masses").
3. Histopathology in Celiac disease
Histopathology in Celiac was first described in 1954 with biopsies from the ileal mucosa. Until now, in the guidelines of the American Gastroenterology Association, it is recommended to take multiple biopsies of the duodenal mucosa for diagnosis.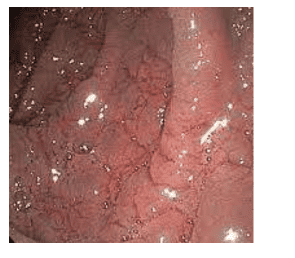
When biopsies of 4 or more pieces were taken, the rate of new diagnoses increased statistically significantly. Targeted biopsies of 1-2 pieces at 9 o'clock or 12 o'clock of the duodenal mucosa in addition to four biopsies of the damaged part of the duodenum increased diagnostic sensitivity to 96%.
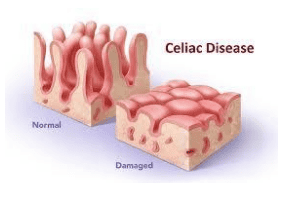
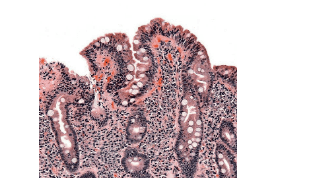
The histopathological findings in Celiac include lymphocytic infiltration in the epithelial layer, thickening of the basement membrane, decreased number of goblet cells, cleft hyperplasia, and atrophy of intestinal villi to varying degrees. In 1992, Marsh published a histopathological classification of lesions on the duodenal mucosal epithelium.
4. Marsh classification for histopathological assessment of Celiac
Level 0: Pre-infiltrate stage: difficult to distinguish from normal mucosa, but IgA, IgM antibody deposition can be detected with a-gliadin Level 1: Infectious stage: epiglottis with infiltrates lymphocytes greater than 30 per 100 enterocytes Level 2: Hyperplastic stage: in addition to infection, the glandular clefts are dilated, the immature epithelial cells proliferate at a rapid rate and appear abundantly. Inflammatory cells Level 3: Destructive phase typical of the intestinal mucosa Grade 4: Atrophic stage with lesions that may not be reversible even with gluten exclusion
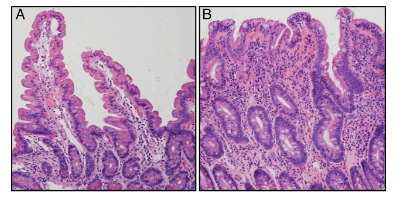
Currently worldwide, the modified Marsh classification is commonly used in which epithelial lymphocyte infiltration is defined as > 40 lymphocytes per 100 enterocytes and Marsh stage 3 is classified into 3 subgroups:
Marsh 3a: lymphocytic infiltration in the epithelial layer, cleft hyperplasia and decreased villi - slit ratio<1:1; Marsh 3b: has atrophic lesions but is still recognizable as villi; Marsh 3c: no longer visible villi.
However, to diagnose Celiac, it is important to note that there are other causes that can lead to atrophy of the villi in the duodenum, including: tropical diarrhea with ulcerative stomatitis - intestinal lesions, overgrowth of bacteria. enteritis, autoimmune enteritis, diarrhea due to hypogammaglobulinemia, drug-induced enterocolitis, Whipple disease, Crohn's disease, eosinophilic enteritis, lymphoma, intestinal tuberculosis, intestinal infection, renal failure nutrition...
5. The role of genetic testing
The most important genetic factor in Celiac is the presence of the genes HLA-D02 and HLA-DQ8. A prospective study of 463 symptomatic patients undergoing small bowel biopsies when Celiac was suspected found that combining HLA-DQ gene testing with serum antibody tests did not increase the accuracy of the test. antibodies alone. Therefore, genetic tests are not routinely used for initial diagnosis. However, in cases where it is difficult to exclude Celiac, this test can be performed including:
Patients with persistent diarrhea but no cause can be found; - Histopathological lesions are uncharacteristic (Marsh I-II) and antibody sera are negative. Evaluation of patients on a gluten-free diet in the absence of previous diagnostic tests; There is a mismatch between serum antibody testing and histopathology; Patients with suspected Celiac disease may relapse into treatment-resistant disease while the initial diagnosis is not clear. Patients with Down: According to one study, the prevalence of Celiac in patients with Down syndrome in the US is estimated to be 10% and HLA-DQ2 is present in 88% of Down cases with positive EMA antibody test and 16% Down patient has a negative EMA antibody test. Negative testing for the HLA-DQ2 and HLA-DQ8 genes can rule out the risk of developing Celiac in children with Down syndrome. Vinmec International General Hospital is a prestigious address trusted by many patients in the implementation of diagnostic and treatment techniques for chronic inflammatory bowel diseases... Along with that, at Vinmec Hospital, the implementation diagnosed through gastrointestinal endoscopy with the Olympus CV 190 endoscope, with the NBI (Narrow Banding Imaging - endoscope with narrow frequency range of light) function, resulting in clearer images of mucosal pathology analysis compared to Conventional endoscopy detects ulcerative lesions in the gastrointestinal tract.
Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can rest assured with the gastrointestinal endoscopy service at the hospital. Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.