Hemorrhoids are a common condition affecting millions of people worldwide, causing symptoms such as pain, itching, and bleeding in the anal area. Many people are unaware of the potential complications and resort to self-treatment at home. Let's delve deeper into this condition with Vinmec.
This article is written under the expert guidance of surgeons from the General Surgery Department at Vinmec Times City International General Hospital.
1. What are Hemorrhoids?
Hemorrhoids involve more than just swollen veins. They are a complex condition affecting a network of blood vessels including small arteries, veins, arteriovenous shunts, smooth muscle, and connective tissue, all lined by normal epithelial tissue of the anal canal. A network of veins lies in the lower layer of the mucosa and is supported by a structure of elastic fibrous tissue. Increased pressure in this area, such as when straining during bowel movements, can cause these veins to swell and form hemorrhoids inside the anal canal. As people age, the supporting connective tissue weakens, and hemorrhoids may begin to prolapse from the anus, leading to internal hemorrhoids.
2. Classification of Hemorrhoids
There are two main types of hemorrhoids: internal and external.
External hemorrhoids develop below the dentate line, also known as the anus-rectal line. They are covered by squamous epithelium and lie just beneath the skin around the anus.
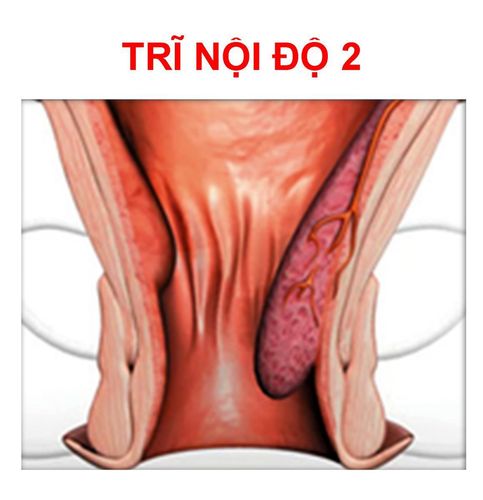
Internal hemorrhoids form above the dentate line and are covered by mucous membrane and transitional epithelium.
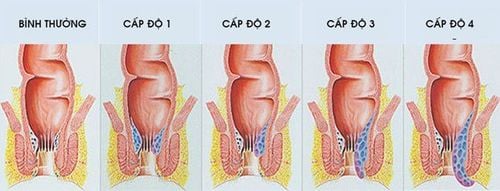
Hemorrhoids are graded based on the degree of prolapse:
- Grade 1: Hemorrhoids are completely inside the anal canal and do not prolapse.
- Grade 2: Hemorrhoids are usually inside the anal canal but may prolapse slightly with straining and then spontaneously reduce.
- Grade 3: Hemorrhoids prolapse with straining, exercise, or when sitting, and must be manually reduced.
- Grade 4: Hemorrhoids are permanently prolapsed.
3. Factors Contributing to Hemorrhoids
Constipation or diarrhea can increase the risk of hemorrhoids, as straining during bowel movements can increase pressure on the veins, leading to stretching and blood congestion. A diet lacking in fiber also contributes to the development of hemorrhoids. Being overweight or obese is another risk factor for hemorrhoids. Heavy labor such as lifting or participating in sports like weightlifting and tennis, as well as activities that require prolonged standing or sitting (like secretaries, tailors, or salespersons), can increase abdominal pressure, hindering blood return to the heart and causing dilation of the rectal veins, which is a contributing factor to hemorrhoids. Pelvic tumors, such as colorectal tumors, uterine tumors, or in cases of advanced pregnancy, can also obstruct blood return to the heart, leading to dilation of the veins and increasing the risk of hemorrhoids.
4. Causes of Hemorrhoids
The veins around the anal area often become strained under pressure, leading to swelling or congestion. Hemorrhoids form when there is increased pressure in the lower rectum due to the following factors:
- Straining during bowel movements.
- Sitting on the toilet for too long.
- Prolonged constipation or diarrhea.
- Obesity.
- Pregnancy.
- Anal sex.
A diet low in fiber.
The risk of hemorrhoids increases with age as the supporting tissue of the veins in the rectum and anus gradually weakens and loses elasticity.
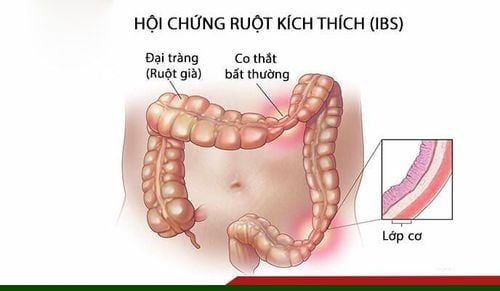
4. Causes of Hemorrhoids The veins around the anus tend to stretch under pressure and can bulge or become congested. Hemorrhoids can develop due to increased pressure in the lower rectum due to:
Straining to have a bowel movement Prolonged sitting on the toilet Diarrhea or chronic constipation Obesity Pregnancy Anal intercourse Low-quality diet Fibroids Hemorrhoids increase with age because the tissue structure that supports the veins in the rectum and anus becomes loose and flabby.

5. Symptoms of Hemorrhoids
Symptoms of hemorrhoids may include:
- Painless bleeding during bowel movements: This is the earliest and most common symptom. Initially, people with hemorrhoids may notice bright red blood on toilet paper or in the toilet bowl. As the condition worsens, bleeding may occur in droplets or streams, and even when sitting.
- Itching or irritation around the anus: This is often caused by mucus secreted from the anal lining.
- Pain or discomfort: People with hemorrhoids often experience discomfort, which can range from mild to severe, due to anal fissures or clots.
- Swelling around the anus.
A lump near the anus: This may be a hemorrhoid with a blood clot, which can be painful and tender.
The symptoms of hemorrhoids often depend on the location of the hemorrhoids:
- External hemorrhoids: These are the most uncomfortable type of hemorrhoids. The skin around the hemorrhoid may become irritated and ulcerated. If a blood clot forms in an external hemorrhoid, the person may experience sudden and severe pain. The patient may be able to feel or see a lump around the anus. This blood clot may be absorbed and leave behind a wrinkled area of skin, causing itching and irritation.
- Internal hemorrhoids: These types of hemorrhoids are usually painless, even when bleeding. People with internal hemorrhoids will see bright red blood on toilet paper or dripping into the toilet bowl. Internal hemorrhoids are usually not visible or palpable and rarely cause discomfort. However, when straining, stool can scratch the surface of the hemorrhoid and cause bleeding. Internal hemorrhoids can also prolapse, becoming protruding hemorrhoids. When prolapsed, hemorrhoids can collect mucus and stool, leading to itching, pain, and irritation. Constant wiping to relieve itching can worsen the condition.

6. Complications of Hemorrhoids
Although complications from hemorrhoids are not common, the following situations can occur:
- Anemia from chronic blood loss: This occurs when the body loses blood through hemorrhoids over a long period, leading to a deficiency in red blood cells needed for oxygen exchange in cells. However, this condition is quite rare.
- Strangulated hemorrhoids: If a hemorrhoid prolapses and becomes trapped, the blood vessels supplying the hemorrhoid can become blocked, causing significant pain. The patient may feel a lump when touched due to a blood clot.
- Thrombosed hemorrhoids: This is a condition where blood clots form in the blood vessels of the hemorrhoid. This often occurs due to dilated blood vessels and blood accumulation, which can be caused by activities such as straining, heavy lifting, pregnancy, or strenuous exercise, increasing abdominal pressure. In the case of external thrombosed hemorrhoids, a small, blue, swollen area can be seen around the anus, often causing pain and a feeling of tightness when touched. For internal thrombosed hemorrhoids, the patient may feel pain and a deep ache, although the symptoms are not as obvious as with external hemorrhoids.
- Perianal dermatitis, papillitis, and fissure: When the skin between the hemorrhoids becomes ulcerated, it can cause itching and burning.
7. Hemorrhoid Treatment
Treatments for symptomatic hemorrhoids include:
7.1 Medical Treatment
For conservative treatment and lifestyle changes, hemorrhoid patients should:
- Increase fiber intake: This is an effective measure for treating bleeding hemorrhoids, along with avoiding irritants like alcohol and chili peppers. Strenuous activities should be limited, and prolonged sitting or standing should be avoided. Adjusting bowel habits to prevent constipation is also important.
- Soaking in a warm bath can relieve discomfort.
- Medication: Patients can use topical creams, suppositories, and other medications to support venous circulation.
7.2 Surgical Treatment
In cases of thrombosed hemorrhoids, early treatment is necessary through surgery using traditional techniques or a combination of clot removal and hemorrhoidectomy using other methods. Other treatment methods for mild hemorrhoids include:
- Rubber band ligation: This is a simple procedure where a rubber band is placed around the hemorrhoid and tightened to cut off its blood supply, causing the hemorrhoid to eventually shrink and fall off. This procedure is suitable for grades 2 and 3 hemorrhoids and has the advantages of being simple, easy to perform, low-cost, and can be performed on an outpatient basis.
- Sclerotherapy: Applied to grades 1 and 2 hemorrhoids, this method is not suitable for external hemorrhoids, thrombosed hemorrhoids, or internal hemorrhoids with inflammation or necrosis. In this procedure, 1-2 ml of a sclerosing agent (such as sodium tetradecyl sulfate or 5% phenol, quinine, urea hydrochloride, polidocanol) is injected with a 25-gauge needle into the submucosa of the hemorrhoid.
- Other advanced surgical methods for hemorrhoids include:
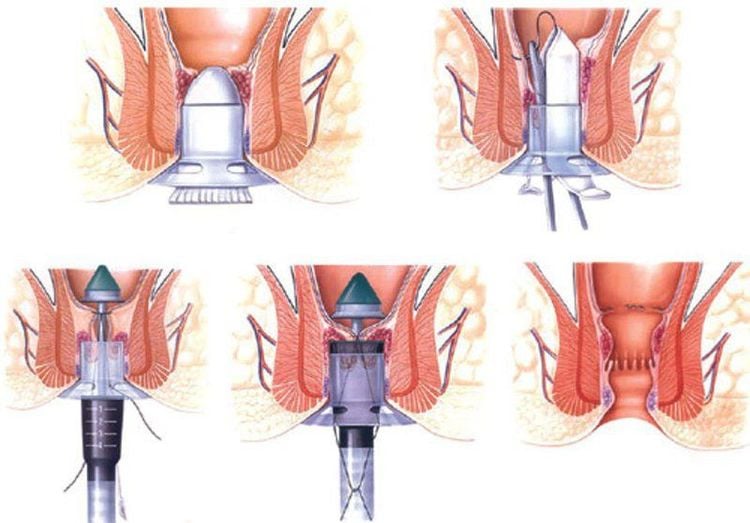
- Longo procedure (stapled hemorrhoidectomy-PPH, 1998): This has been accepted in many European and Asian countries. It is a popular choice for the surgical treatment of grade 3 and 4 internal hemorrhoids. In China, over the past decade, this method has even tended to replace traditional hemorrhoidectomy. This method does not directly cut the hemorrhoids but relies on the principle of interrupting the blood supply to the upper and middle hemorrhoids, then suturing the prolapsed anorectal mucosa upwards, helping the hemorrhoids return to the anal canal, thereby causing the hemorrhoidal tissue to atrophy. The advantage of this method is that it causes less discomfort as it does not require cutting the skin around the anus.
- Doppler-guided hemorrhoidal artery ligation (THD): Performed under ultrasound guidance, this procedure blocks the blood supply to the hemorrhoidal arteries, reducing hemorrhoidal swelling.
- Traditional hemorrhoidectomy methods such as Milligan-Morgan, Ferguson, and Whitehead often directly intervene in the hemorrhoid and can be painful.
Precautions for hemorrhoid treatment:
Surgery is not recommended for patients with weak immune systems or those with active forms of colitis. Emergency hemorrhoid surgery is associated with a higher rate of complications. Acute complications of hemorrhoid surgery include pain, wound infection, recurrent bleeding, and urinary retention. Some patients may experience late complications such as loss of bowel control due to damage to the anal sphincter during surgery.
8. Hemorrhoid Prevention
The most effective way to prevent hemorrhoids is to maintain soft stools that can easily pass through the anus. Here are some recommendations to prevent hemorrhoids and reduce symptoms if you already have them:
Increase fiber in your diet: Incorporate plenty of fruits, vegetables, and whole grains such as wheat, oats, barley, corn, brown rice, rye, and millet to soften stools and increase stool bulk. Start increasing fiber gradually to avoid excessive gas.

- Stay hydrated: Aim to drink six to eight glasses of water or other fluids daily to help soften stools.
- Increase fiber intake: Most people don't get enough fiber. Aim for 25 grams daily for women and 38 grams for men. Over-the-counter fiber supplements like Metamucil and Citrucel can help reduce symptoms and bleeding. However, ensure you drink plenty of water to prevent constipation.
- Avoid straining: Straining can increase pressure on the veins in the lower rectum, causing hemorrhoids to swell and bleed.
- Don't ignore the urge to defecate: Delaying bowel movements can lead to harder, drier stools.
- Stay active: Regular exercise can prevent constipation and reduce pressure on veins. It can also help with weight management.
- Avoid prolonged sitting: Sitting for long periods, especially on the toilet, can increase pressure on the veins in the anus.
Remember: Soft stools are key to preventing hemorrhoids. A diet rich in fruits, vegetables, and whole grains, combined with adequate hydration, is essential.
Important note: Many people, especially those over 40, attempt to self-treat hemorrhoids without consulting a doctor. This can be dangerous as rectal bleeding can be a symptom of other conditions, both benign and malignant, such as colorectal cancer, anal cancer, and colorectal polyps. Additionally, hemorrhoids can be a symptom of other underlying health issues.
If you notice any changes in your bowel habits, stool color, or if you experience bleeding accompanied by pain, frequent bleeding, or severe bleeding that does not improve after using medication, you should contact your doctor immediately for advice and a proper diagnosis. In particular, if you have severe rectal bleeding accompanied by symptoms such as dizziness, lightheadedness, or fainting, you should go to the hospital immediately.
If you need specialized consultation and examination, you can contact any Vinmec Health System hospital nationwide. For your convenience, you can book an appointment online through the hospital's website.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.