This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Colorectal cancer is a dangerous cancer with a low prognosis. Compliance with colorectal cancer screening will provide a better chance of detection and treatment.
1. As recommended by the American Gastroenterology Association (ACG)
The authors suggest organized screening programs to improve compliance with colorectal cancer screening compared with opportunistic screening. The authors suggest the following strategies to improve screening adherence: patient navigation, patient reminders, clinician interventions, provider recommendations, and decision support tools clinical.
2. Organized colorectal cancer screening
Colorectal cancer screening is a process that occurs in a multi-level healthcare setting. The International Agency for Research on Cancer defines an organized screening program as one that has the following characteristics:
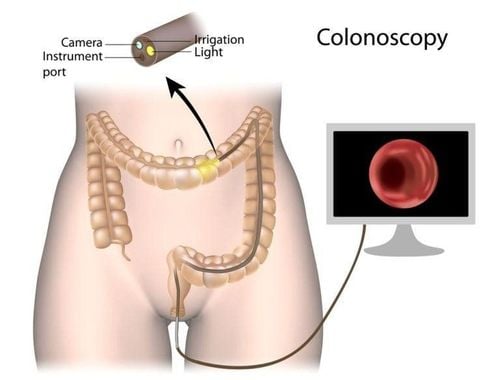
A clear policy with specific age categories, methods and time periods for screening ; A defined target population; A management team is responsible for implementation; A healthcare team for decision making and care; (v) quality assurance structure; A method for determining the occurrence of cancer in a population. In contrast, opportunistic screening is performed outside of an organized screening program, usually through reimbursement of physicians' service fees. Compared to opportunistic screening, organized screening focuses more on the quality of the screening process, including the follow-up of participants. In the United States, screening is primarily opportunistic, and among those screened updated in the 2010 National Health Interview Survey data, colonoscopy is the most commonly reported test. (54.6%), followed by flexible colonoscopy and fecal occult blood test (8.8%). Insurance status is the single most important determinant of colorectal cancer screening. In the 2000–2005 National Health Interview Survey study, Trivers et al showed that in adults 50–64 years of age, the reported prevalence (incidence [95% CI]) for occult blood tests stool or colonoscopy over the years was 41.5% (39.3%–43.7%) in patients with private insurance, 31.2% (24.2%–39.1%) in those with people with public insurance and 16.1% (11.9%–21.4%) among those without insurance.

3. Higher rates of screening reported with organized screening compared to opportunistic screening
In the PASSI study in Italy, Carrozzi et al showed that out of a total of 38% of those who reported being screened, 31% of those enrolled in an organized screening program compared with 7% of those who were screened. opportunity filter. A successful example of organized colorectal cancer screening in the United States is the Kaiser Permanente Northern California integrated health system. In that system, which serves about 4 million members, before 2006, colorectal cancer screening was opportunistic, primarily using sigmoidoscopy and fecal occult blood testing. Beginning in 2007, screening shifted to a postal fecal occult blood test approach in individuals who were not up-to-date. Reach screening includes mail, secure e-mail, and phone reminders.
In addition, reminders for providers have been added to the electronic medical record. A recent study reported that colorectal cancer screening rates increased from 38.9% in 2000 to 82.7% in 2015. Another successful example of organized colorectal cancer screening U.S. institutions with approximately 80% screening rates are Veterans' health care systems, with new use of provider alerts and other electronic health care reminders and processes required. followed when inviting individuals for screening.
4. Interventions to enhance screening compliance
At the screening organization level, small media interventions to raise awareness (e.g., brochures) and invitations/reminders are associated with increased engagement, also as support for scheduling and booking appointments. A recent systematic review and meta-analysis of interventions aimed at enhancing colorectal cancer screening by any of the recommended modalities in the United States reported that access to hidden blood testing fecal occult blood test (i.e. active delivery of fecal blood tests), patient navigation, patient reminders, clinician intervention in detailed learning and prompts of Clinicians are associated with increased rates of colorectal cancer screening comparing fecal occult blood test acceptance rates in 3 groups: invitation alone, invitation plus notification, and the last two groups along with an information booklet about colorectal cancer and screening.
Absorption rate of fecal occult blood test was highest in the group that received all 3 letters (reception rate: notice + invitation: 59%, notice + brochure + invitation: 58.5 % and invitation-only group: 53.9%, P < 0.001). Furthermore, adding a fecal occult blood test in a mailer versus a letter or invitation alone increases screening rates but leads to increased costs.
5. The role of the health care provider
At the provider level, primary care provider or general practitioner (GP) involvement is associated with increased participation in organized screening facilities and festival. A recommendation to get screened from a primary care provider who is clearly known and trusted by that person is effective in increasing participation.
A cluster randomized controlled study conducted in France in the context of organized screening found that providing GPs with a list of their patients not yet screened for colorectal cancer resulted in a slightly increased screening for fecal occult blood at 1 year. The between-group difference was 4.2% (95% CI 2.3%–6.2%) for the patient-specific reminder group compared with the usual care group.
A cluster randomized controlled study conducted at federally qualified medical centers in the United States found that clinics have an electronic health record embed tool (letters of referrals, reviews, etc.) Postal fecal occult blood tests, reminder letters) had a higher screening participation rate (18.3% vs 14.5%, difference 3.8% points, 95% CI 0.6 %–7.0%) compared with usual care.

6. Recommendations for colorectal cancer screening
A systematic review reported that in organized programs, invitations, especially if signed by GPs, and reminder letters for non-participants increased in attractiveness. . In addition, communication between patients and doctors also affects screening acceptance rates. In a randomized controlled study, Boguradzka et al showed higher participation rates among patients who were consulted by their primary care physician for colorectal cancer screening compared with those who received get an information leaflet (47% vs 13.7%). In an observational study in Kaiser Permanente Northwest, Mosen et al. found that physician explanations (OR 1.27; 95% CI 1.03–1.58) and physician encouragement were greater (OR 6.74; 95% CI 3.57–12.72) was associated with endoscopy.
In this study, they also found that patients who reported relatively little/more doctor's encouragement were 6 times more likely to receive a fecal occult blood test than patients who reported no /slightly recommended (OR 6.54; 95% CI 2.76–15.48).
7. Patient navigation and reduction of structural barriers also enhance screening uptake
Muliira et al reviewed 15 studies, finding that a patient navigator improved the reception of colorectal cancer screening by rates ranging from 11% to 91%. Patient navigation is most effective in minority patients. However, in a randomized trial, Lairson et al found that navigating was associated with an increased cost (patient navigation intervention: $289 versus standard intervention: $167). Reducing structural barriers such as providing extended or non-standard clinic hours have also been shown to be effective strategies. For colonoscopy reception, peer training (recommended from a volunteer patient who had undergone prior colonoscopy) was associated with increased absorption compared with a submitted brochure by mail in a study in the United States.
8. Clinicians and patient reminder systems also influence colorectal cancer screening acceptance
In a randomized controlled study, Hirst et al showed higher absorption of fecal occult blood tests in patients who received written reminders compared with those who received usual care. . In a randomized controlled study of 8 primary care clinics in Florida, Roetzheim et al reported increased fecal occult blood test completion rates (OR 2.5; 95% 1.65–4). ) with the intervention of screening and flagging medical charts due to screening and having an office responsible for arranging screening tests for patients.
9. The authors suggest the following strategies to improve adherence to active screening test follow-up: Mail and phone reminders, patient navigation, and provider intervention
In a retrospective cross-sectional study, May et al found that among 347 veterans (37.9%) who did not undergo follow-up colonoscopy, the reason was patient related (49 .3%), vendor related (16.4%), system related (12.1%) or multifactorial (22.2%). Interventions including health education leaflets, patient reminders, seminars, and helplines have been found to increase completion rates for patients with positive screening results. In a project of the Department of Health Promotion in Taiwan, Chang et al. showed that after making health education leaflets, sending reminders to patients for follow-up visits, organizing seminars, opening consultation lines, The rate of completion of endoscopy evaluating patients with positive screening increased from 53.63% to 66.08%. Mail or phone prompts have been shown to increase follow-up rates of screen-positive patients. In the Study Promoting Adherence to Colonoscopy Referrals, Zorzi et al reported that participation rates after initial invitation by mail and by phone were similar (86.0% vs 84). .0%, RR: 1.02; 95% CI 0.97–1.08); among those who did not respond to the initial invitation, the compliance rate with a specialist appointment recall was 50.4%, significantly higher than with a mail-in recall (38.1%; RR : 1.33; 95% CI 1.01–1.76) or in person - face-to-face consultation with a general practitioner (30.8%; RR: 1.45; 95% CI 1.14–1 ,eighty seven).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Shaukat, Aasma MD et al. ACG Clinical Guidelines: Screening for Colorectal Cancer 2021. American Journal of Gastroenterology: March 2021 - Volume 116 - Issue 3 - pp. 458-479