This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
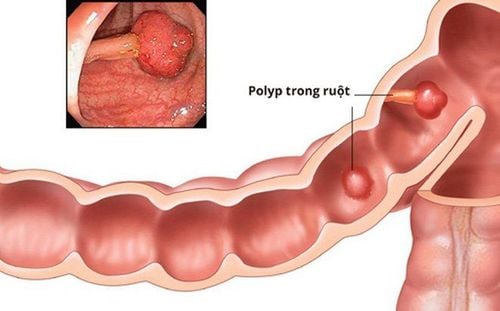
Poverty has become a barrier to colorectal cancer screening, especially in under-resourced countries. Patients are unlikely to seek preventive services when they cannot meet their basic needs. The effects of the COVID-19 pandemic could worsen these barriers and lead to a reduction in screening capacity in these populations.
1. The impact of the COVID-19 pandemic has also exacerbated patient barriers to receiving care.
The impact of the pandemic causes significant psychological stress on patients and can affect their desire to seek cancer preventive care. In the United States, as unemployment rises, many workers and their dependents are at risk of losing employer-based coverage, which will reduce access to services. this preventive health care. Even people with health insurance may not want to seek services for fear of being exposed to COVID-19. In addition, those unable to use telehealth options are further restricted in accessing care. Patients residing in lower income zip codes or in minority populated areas have lower rates of telemedicine usage. Older adults and those living in rural areas may also lack the technology needed to access telemedicine.
2. Long-term outcomes of colorectal cancer screening in the era of covid-19
The discontinuation of colorectal cancer screening has resulted in a large number of patients waiting for screening tests. As the pandemic is still affecting many major countries around the world, screening is unlikely to return to full capacity in the near future. A build-up of a backlog coupled with an inability to continue with full screening can have significant consequences.
3. There are disparities in colorectal cancer data across racial and ethnic groups
Prior to COVID-19, there were disparities in colorectal cancer data across racial and ethnic groups as well as in patients with low socioeconomic status in the United States. Colorectal cancer rates are highest among non-Hispanic blacks and AI/ANs. From 2012 to 2016, the highest age-adjusted incidence of colorectal cancer in non-Hispanic blacks was 45.7 and AI/ANs was 43.3 per 100000 people. The difference in colorectal cancer mortality among non-Hispanic blacks compared with other racial and ethnic groups is more remarkable. From 2013 to 2017, non-Hispanic blacks had a 40% higher mortality rate than non-Hispanic whites, with the death rate among non-Hispanic blacks Hispanic is 19.0 compared with 13.8 for non-Hispanic whites. Mortality rate in non-Hispanic blacks is more than twice that of Asian Americans/Pacific Islanders, who have a mortality rate of 9.5 per 100,000 in Americans / Pacific Island.
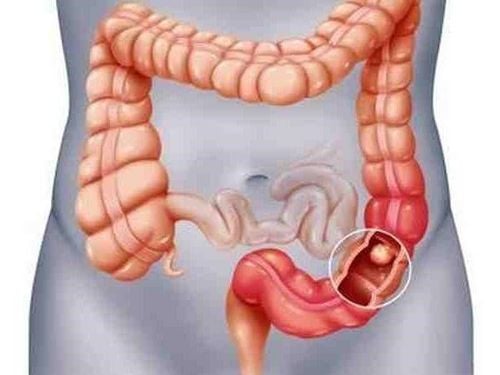
4. Patients who have low socioeconomic status also affect colorectal cancer rates.
A prospective analysis by the US National Institutes of Health-Retirement Diet and Health Research Association from 1995 to 1996 of more than half a million adults found that the incidence of cancer Overall colorectal cancer was significantly higher in those with low education or in patients living in the vicinity of low socioeconomic status. This association persisted after accounting for individual colorectal cancer risk factors such as sex, age, race and ethnicity, residency status and history of colorectal cancer at grade level. first relativity.
Adults with less than 12 years of education have a 42% higher risk of colorectal cancer and those living in the poorest neighborhoods have a 31% higher risk of colorectal cancer. When comparing rural and urban neighborhoods, the rural population also has an increased incidence and mortality from colorectal cancer. The basis for these disparities is complex and multifactorial. Further analysis of data from the US National Institutes of Health-Association for the Study of Diet and Retirement's Health found 44% of the association between education and 36% of the association between regions. low socioeconomic status populations The low incidence of colorectal cancer is due to a combination of health behaviors (diet, physical activity, and smoking) and only body mass number.
5. Other barriers to colorectal cancer screening
Other barriers to colorectal cancer screening that contribute to disparities include lack of health insurance, inability to take time off work for colonoscopy, cost, lack of provider referrals severity, the discomfort of colorectal cancer screening tests (fecal sampling and storage and bowel preparation for colonoscopy), and the lack of options offered for screening tests that only endoscopy provided. Among non-Hispanic blacks, there is a lack of knowledge about colorectal cancer and mistrust of the medical community. In one study, only 38% of non-Hispanic blacks thought colorectal cancer was often fatal, 40% did not feel the disease was preventable, and 43% did not think there was a cause. out colorectal cancer. COVID-19 may exacerbate these inequalities.

6. Medically underserved population groups have limited access to health services
Medically underserved populations had limited access to pre-pandemic preventive health services and an estimated 86% decrease in colon cancer screening over the period from January 20, 2020 to April 21, 2020. In the United States, federally qualified medical centers are federally funded community health centers (CHCs). Federally qualified medical centers provide preventive services to more than 22 million low-income, uninsured and/or uninsured Americans. There has been a significant reduction in the number of clinical visits and the availability of endoscopic services for these patients. Additionally, clinics that offer fecal immunohistochemistry/FOBT pickup and drop-off have suspended colorectal cancer screening due to social distancing policies. In the United States, telemedicine usage rates are also lower among patients residing in lower-income areas or in minority populations, which may indicate further limitations. in accessing health care services.
7. Adapting to growing colorectal cancer inequality
Disruptions to health services due to COVID-19 could cause further stress in medically underserved populations that have limited access to preventive health services even before the pandemic. There are several proposals proposed to counteract the decline in colorectal cancer screening for these patients. Stool immunohistochemistry and FOBT kits are mailed and initiating safety protocols for receiving and returning these kits have been recommended. Patients with abnormal fecal immunohistochemistry/FOBT or who develop symptoms at intervals associated with colorectal cancer should have priority follow-up and colonoscopy. Telemedicine visits can be used to monitor these patients.
At the beginning of the pandemic, some insurance centers in the US expanded coverage and payment for telehealth services. This can significantly increase access to care, as telemedicine allows patients to be more flexible with their appointments, limit travel time, and cut time and costs. travel expenses.
8. The success of remote services
A study of four major centers in Southern California shows success in telehealth with 80%-85% of their clinical consultations shifting to telehealth as of March 2020 with few missed appointment. With regard to endoscopy for these patients, advocacy programs are encouraged to create a list of community gastroenterologists to provide endoscopy for CHC patients. A qualitative study from Mexico found that the implementation of screening programs that offer free fecal immunochemical testing and colonoscopy significantly increases colorectal cancer screening participation. To reduce knowledge gaps in patients, existing platforms should provide information about COVID-19 and expand colorectal cancer awareness throughout the year. Advocacy campaigns and advocacy for underserved communities should use virtual platforms to continue efforts amid COVID-19. While these changes are inherently difficult to organize during the COVID-19 leisure time, implementing them now can help address these disparities and prevent their exacerbation. It will be hugely beneficial to make fecal immunohistochemistry and FOBT kits more accessible by mail, increase the convenience of remote systems, and disseminate virtual information in an increasingly online world. for these patient populations.
9. Effect of new screening guidelines on recovery efficiency
In October 2020, the Foundation for Disease Control and Prevention drafted a recommendation to begin colon cancer screening at age 45 rather than at age 50 as previously recommended. This new recommendation is in line with recommendations from the American Cancer Society, which lowered the recommended age for screening from 50 to 45 in June 2018. According to the American Foundation for Disease Control and Prevention, screening Colorectal cancer for people aged 45-49 is a category B recommendation, which means there is strong evidence that there is a true mean benefit or moderate evidence that there is a significant benefit.
Meanwhile, screening for people aged 50-75 is a category A recommendation, which means there is a high degree of certainty that there is a significant benefit. This new recommendation would make more than 20 million Americans, ages 45-50, eligible for screening. This adds up to 20 million people waiting for colorectal cancer screening in addition to the COVID-19-related backlog whose screening has been halted. This further increases the need for a new public health strategy to ensure that those at highest risk of colorectal cancer are prioritized for screening. If resources are not distributed appropriately, there is a risk of diverting health care resources away from those with high risk factors and alarming symptoms. This problem can be addressed by using noninvasive stool-based screening tests and stratifying the patient's risk based on individual risk factors and the presence of alarming symptoms. motion.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.