This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalOther concomitant risk factors must also be considered before concluding that gastric mucosal ectopic and esophageal cancer is associated with esophageal cancer, since in such patients it is possible that the cancer of the esophagus is true. due to comorbidities, not ectopic gastric mucosa.
1. Current diagnosis of this disease
Ectopic gastric mucosal structures are largely considered asymptomatic or relatively unimportant. Recently, more and more symptoms have been reported to be associated with these esophageal lesions, making them a subject of controversy.Currently, there are no standard guidelines for the management of esophageal ectopic gastric mucosal symptoms. In particular, the diagnosis of the condition through the use of a longer extubation time combined with the routine use of optical endoscopy in the esophagus may be useful to further explore the significance of these structures. misplaced gastric mucosa.
2. Ectopic and cancerous gastric mucosa
Another related question is whether ectopic gastric mucosal structure is involved in the pathophysiology of esophageal cancer? Considering the number of studies reporting an ectopic gastric mucosal structure as a harmless mucosal region that can be overlooked, one might think that the limited number of cases with both esophageal and Ectopic gastric mucosal structures are incidental.On the other hand, recent case reports of adenocarcinoma describe ectopic gastric mucosal structures as small and flat lesions and rather conspicuous compared with ectopic gastric mucosal structures. healthy place. Therefore, should endoscopists feel guilty for omitting this type of lesion or for not taking biopsies frequently? The answer to this question depends on how much the lesion is related to the patient's symptoms and if the lesion affects the patient's outcome.
3. Factors associated with both patients with ectopic gastric mucosa and esophageal cancer
Other concomitant risk factors must also be considered before concluding that gastric mucosal ectopic and esophageal cancer is associated with esophageal cancer, since in such patients it is possible that the actual cancer is true. management is due to comorbidities, not ectopic gastric mucosa.A recent study found no differences related to age, race, household income or waist-to-hip ratio, while patients with ectopic gastric mucosal disease had heavier smoking history (mean 23.7 packs/year vs 16.3 packs/year, P = 0.006). There was no significant difference compared to those who never smoked. No association was found between weekly alcohol intake and ectopic gastric mucosal structure. A recent report of a large 14-year population study analyzing whether ectopic gastric mucosal structures were significantly associated with proximal esophageal adenocarcinoma revealed only 39 cases diagnosed. simultaneously from their literature review and only 3 additional cases during their study. Indeed, the authors also mention that the lack of reports of ectopic gastric mucosal structures in the endoscopic report may be a limitation of these studies.
In 2013, Chong et al was able to find only 43 cases of esophageal cancer in the literature with concomitant presentation with ectopic gastric mucosa since 1950 when Carrie et al. reported the first case. .
Furthermore, Sahin et al found no cases of adenocarcinoma or dysplasia and only additional intestinal metaplasia was detected in 5 out of 123 cases of ectopic gastric mucosal structures.
4. Should all ectopic gastric mucosal lesions be biopsied?
The lack of long-term follow-up studies of ectopic gastric mucosal structures may be a source of this deviation. Other authors such as Peitz et al also suggested that the incidence of ectopic gastric mucosal structures was underestimated, making it difficult to correlate with advanced cervical esophageal cancer. Because of the rare frequency of preeclampsia reported for ectopic gastric mucosal structures, the authors do not advocate routine biopsies to determine its histopathology, but targeted biopsies should be considered. whenever any abnormalities are observed in the area. In addition to this opinion, there are technical difficulties in the region that is commonly located in the upper esophagus (spasm of the upper esophageal sphincter or low tolerance of the patient with no progress), because Therefore, routine biopsies should be limited to sites that are atypical of gastric mucosal structures that are ectopic (eg, distal or medial portion of the esophagus) or appear atypical (eg, polypoid type).
5. The role of new imaging techniques in the evaluation of gastric mucosa ectopic
For symptomatic patients with ectopic gastric mucosal structures that are often localized and when biopsies cannot be confirmed, virtual staining endoscopy with selected follow-up cases may be helpful.Ambient laser endoscopy can avoid both physician and patient anxiety about the prediction associated with getting the correct diagnosis. Unfortunately, the feasibility of this technique for general use is impaired due to increased costs and limited accessibility.
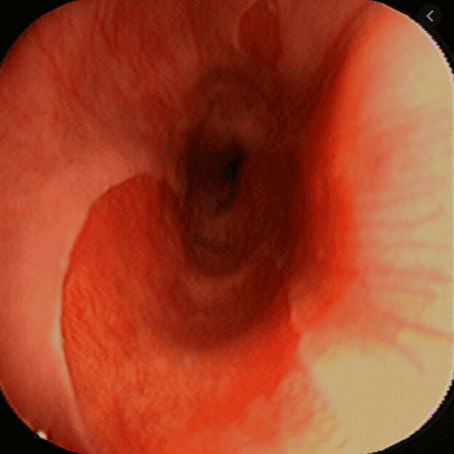
Detection of ectopic gastric mucosa-like lesions and subsequent histological confirmation will help avoid confusion between primary cancer and mucosal foreign bodies. Ectopic gastric mucosal structures appear with salmon-red or salmon-pink focal areas on standard endoscopy and are a well-demarcated homogeneous dark brown lesion with pale green squamous epithelium in NBI mode.
>> See more: Treatment and screening for ectopic gastric mucosa in the esophagus - Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
6. Role of NBI . Narrowband Imaging System
The NBI system can be very useful to identify brown areas with brown dots and branching vessels in the cervical esophagus as potential superficial esophageal cancer. Therefore, the combined application of magnification and NBI can help inform and direct the management of diagnosis and early detection of esophageal cancer. Magnified endoscopy with NBI system is superior to conventional white light endoscopy in detecting early cancer and helping to resolve the microvascular tissue of the esophageal mucosal surface. Ideally, it would be possible to deploy in the future an automated early cancer detection system similar to the automated computer algorithm developed for Barrett's esophagus by Fons van der Sommen et al. propose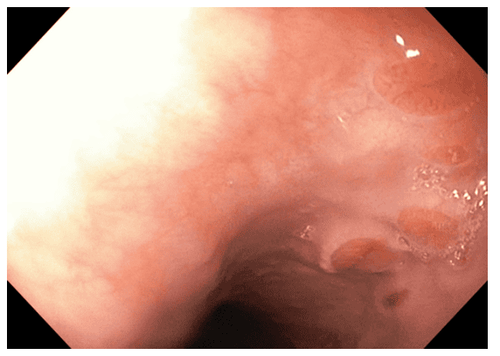
7. Does ectopic gastric mucosal structure increase the risk of esophageal carcinoma?
Whether ectopic gastric mucosal structures increase the risk of esophageal carcinoma is controversial. Acid secretion is also a suspected cause of malignancy, but there is a difference between the prevalence of ectopic gastric mucosal structures associated with symptomatic acid and rare cases of malignancy. reported.There may be other concomitant risk factors involved. However, considering that cancers in ectopic gastric mucosal structures are often reported as isolated cases, focus should be on being able to accurately distinguish between anomalous gastric mucosal structures and ectopic gastric mucosal structures. malignant and superficial malignancies. Since white-light endoscopy may not reveal abnormal features of early cancer, the routine use of virtual esophagogastroduodenoscopy in the esophagus is justified. Misreporting of the incidence of ectopic gastric mucosal structures by endoscopy must be avoided and future studies should be performed to draw more appropriate conclusions.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, diseases that cause chronic diarrhea, Crohn's disease, gastric mucosa Esophageal ectopic... Along with that, at Vinmec Hospital, screening for gastric cancer and gastric polyps is done through gastroscopy with Olympus CV 190 endoscope, with NBI (Narrow) function. Banding Imaging - endoscopy with narrow light frequency) results in clearer images of mucosal pathology than conventional endoscopy, detecting ulcerative colitis lesions, digestive cancer lesions In the early stages... Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can be assured of endoscopy services. stomach, esophagus at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferenceRaine CH. Ectopic gastric mucosa in the upper esophagus as a cause of dysphagia. Ann Otol Rhinol Laryngol. 1983; 92 :65-66. [PubMed] [DOI] Truong LD, Stroehlein JR, McKechnie JC. Gastric heterotopia of the proximal esophagus: a report of four cases detected by endoscopy and review of literature. AmJ Gastroenterol. 1986; 81:1162-1166. [PubMed] Akbayir N , Alkim C, Erdem L, Sökmen HM, Sungun A, Başak T, Turgut S, Mungan Z. Heterotopic gastric mucosa in the cervical esophagus (inlet patch): endoscopic prevalence, histological and clinical characteristics. J Gastroenterol Hepatol. 2004; 19:891-896. [PubMed] [DOI] Borhan-Manesh F , Farnum JB. Incidence of heterotopic gastric mucosa in the upper oesophagus. Gut. 1991; 32 :968-972. [PubMed] [DOI] Tang P , McKinley MJ, Sporrer M, Kahn E. Inlet patch: prevalence, histologic type, and association with esophagitis, Barrett esophagus, and antritis. Arch Pathol Lab Med. 2004; 128 :444-447. [PubMed] [DOI] Adriana Ciocalteu, Petrica Popa, Issues and controversies in esophageal inlet patch, World J Gastroenterol. Aug 14, 2019; 25(30): 4061-4073