This is an automatically translated article.
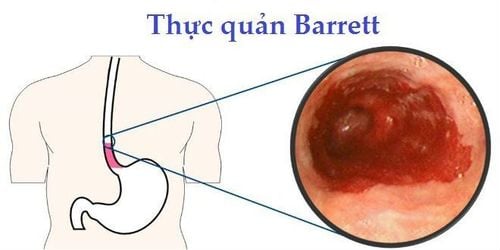
The article is professionally consulted by Master, Doctor Tran Ngoc Hai - Internal Oncologist - Internal Oncology Department - Vinmec Times City International Hospital.Barrett's esophagus is a disease of the digestive system that occurs when the cells in the lining of the esophagus become abnormal, which can lead to esophageal cancer.
1. What is Barrett's esophagus?
With Barrett's esophagus, the cells in the esophagus (the tube connecting the mouth to the stomach) are replaced by cells similar to the lining of the intestines.This disease is usually diagnosed in people who have persistent gastroesophageal reflux disease (GERD). However, only a small percentage of GERD patients will develop Barrett's esophagus.
Barrett's esophagus is associated with an increased risk of progression to esophageal cancer. Although this risk is relatively small, patients should still be checked regularly for the presence of precancerous cells. If precancerous cells are detected early, they can be treated in time to prevent esophageal cancer.

Barrett thực quản làm gia tăng nguy cơ bị ung thư thực quản
2. Barrett's esophagus symptoms
Changes in cells in the lining of the esophagus usually cause no symptoms. Instead, Barrett's esophagus symptoms that patients experience mainly stem from gastroesophageal reflux conditions, including:Heartburn, frequent heartburn; Difficulty swallowing food; Chest pain (uncommon). Many people with Barrett's esophagus do not show any symptoms.
3. When to see a doctor?
If you experience discomfort with heartburn and acid reflux for more than 5 years, ask your doctor about the risk of Barrett's esophagus. See your doctor as soon as possible if you notice:Chest pain, possibly a symptom of a heart attack; Difficulty swallowing; Vomiting blood or liquid that looks like coffee grounds; Passing black or bloody stools.
4. Causes of Barrett's esophagus
The exact cause of Barrett's esophagus is not known. However, statistics show that most people with the disease have symptoms of chronic acid reflux.
Acid reflux from the stomach back into the esophagus, leading to damage to the esophageal tissue. As the esophagus tries to heal itself, the cells in the lining may have changed its nature and structure and caused Barrett's esophagus.
Despite this, some patients diagnosed with Barrett's esophagus do not have heartburn or acid reflux.
5. Risk factors
Factors that increase the risk of Barrett's esophagus include:Chronic heartburn and acid reflux: Patients with GERD that do not get relief with medication or require regular medication are at increased risk for Barrett's esophagus. ; Advanced age: Barrett's esophagus can occur at any age, but is more common in older adults; Male gender: Statistics show that men are more likely to get the disease than women; Being Caucasian: White people are at higher risk than people of other races; Being overweight: Excess fat around the abdomen increases the risk of disease; Has a habit of smoking.

Thường xuyên ợ nóng và bị trào ngược axit dạ dày - thực quản có nguy cơ cao mắc Barret thực quản
6. Complications of Barrett's esophagus
Patients with Barrett's esophagus have a higher risk of esophageal cancer than the general population. However, the overall risk is still low, even in people who have found precancerous cells in their esophagus.
7. Diagnosis of disease
7.1. Diagnostic method
Endoscopy is the most commonly used method to determine if a patient has Barrett's esophagus.
A small tube with a lighted camera is passed through the patient's throat to check for signs and symptoms of Barrett's esophagus. Normal esophageal tissue looks pale and glossy. Meanwhile, patients with Barrett's esophagus, the tissue in this organ is dark red.
In addition, the doctor will remove a piece of tissue (biopsy) to examine and determine the extent of the change.
7.2. Determine the degree of tissue change
The doctor performs a laboratory tissue test (pathology study) to determine the degree of dysplasia in the patient's sample of esophageal cells. The diagnosis of esophageal dysplasia is often difficult, so it is best to have two doctors, including at least one who specializes in digestive pathology, agree on the final diagnosis. Accordingly, the possible conclusions are:
No dysplasia: If the patient has Barrett's esophagus but no precancerous signs are detected; Low-grade dysplasia: If some cells have precancerous signs (mild level). Severe dysplasia: If the cells show signs of large abnormalities associated with esophageal cancer. Severe dysplasia is thought to be the final stage before it turns into esophageal cancer.
7.3. Barrett's esophagus screening
Risk screening is generally recommended for men with at least one GERD symptom, unresponsive to drug therapy (proton pump inhibitors), and at least two other risk factors, including include:
Over 50 years old; Be white; Have a lot of belly fat; Being a smoker; Have a family history of Barrett's esophagus or esophageal cancer. Although women are less likely to have Barrett's esophagus, they should still be screened if they have symptoms of difficult-to-manage acid reflux or other risk factors for Barrett's esophagus.
8. Treatment of Barrett's esophagus
Treatment for patients with Barrett's esophagus depends on the extent of the abnormal cells in the esophagus and the patient's overall health.
8.1. Cases without dysplasia
Indications for possible treatment are:
Routine endoscopy to monitor and examine cells in the esophagus. If the biopsy results show no dysplasia, the patient is likely to have a follow-up endoscopy one year later and, if no change occurs, repeat after 3 years; Treatment of GERD: Medication and lifestyle changes can reduce a patient's signs and symptoms. Surgery may also be an option. Treating GERD cannot resolve underlying Barrett's esophagus and does not reduce the risk of esophageal cancer, but makes it easier for doctors to detect dysplasia.
8.2. Low grade dysplasia
For low-grade dysplasia, your doctor may recommend a repeat endoscopy within 6 months, with additional follow-up every 6-12 months.
However, for patients at risk for esophageal cancer, preferred treatments include:
Laparoscopic surgery: Using an endoscope to remove abnormal cells; Radiofrequency Abnormal Cell Cauterization: Uses heat to remove abnormal esophageal tissue. Methods may be recommended after laparoscopic surgery.
8.3. Severe dysplasia
High-grade dysplasia is thought to be a precursor to esophageal cancer. For this reason, your doctor may recommend laparoscopic surgery or radiofrequency ablation. Other treatment options include:
Cryotherapy: Using an endoscope to deliver liquid or cold air to abnormal cells in the esophagus. The cells can be rewarmed and then frozen again. Cycles of freezing and thawing will damage abnormal cells; Photodynamic therapy: Destroying abnormal cells with light energy; Esophageal surgery: Removing the damaged part of the esophagus, the rest is connected to the patient's stomach. Relapse of Barrett's esophagus sometimes occurs after treatment. Therefore, the doctor will usually recommend the patient to have regular follow-up check-ups.
Master. Dr. Tran Ngoc Hai has experience in examination, diagnosis and treatment of cancers, including 15 years working at the Oncology Center of Bach Mai Hospital. Currently, he is an Internal Oncologist at the Radiation Oncology Center - Vinmec Times City International Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: mayoclinic.org
MORE:
Barrett's esophagus may increase the risk of esophageal cancer Treatments for Barrett's esophagus Esophageal cancer: Causes, symptoms, prognosis and how to treat