This is an automatically translated article.
The article is written by Master, Doctor Le Thai Bao - ICU Doctor - Intensive Care Department - Vinmec Times City International Hospital
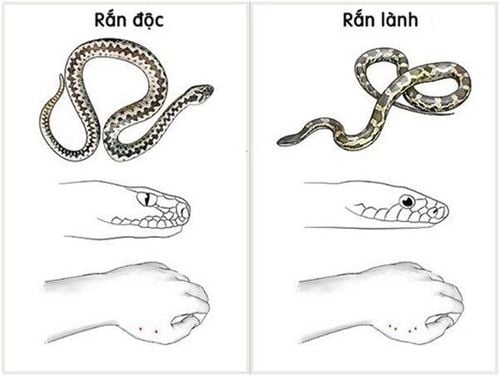
If first aid when bitten by a venomous snake is not done properly, the victim is at risk of gangrene, blood infection, or even death. The immobilization of the bitten limb, which slows the onset of symptoms of toxicity, especially paralysis, may be enough to help the patient reach the nearest medical facility safely.
1. Outline
Venomous snake bites are the most common type of animal poisoning. Venomous snake bites can be fatal on the way to the hospital.
Snake venom from the bite site to the systemic circulation mainly via the lymphatic route.
Compression bandage immobilizes the bitten limb to create pressure to slow down the process of venom traveling through the lymphatic system to the systemic circulation, and at the same time immobilizing the bitten limb to limit muscle contraction thereby also reducing the pumping role muscle blood with return limb circulation. These effects, which slow the onset of symptoms of toxicity, especially paralysis, may be sufficient to enable the patient to safely reach the nearest medical facility.
Indications : Cases of being bitten by scorpions, kraits, king cobras, and cobras.
Contraindications : Types of viper bites.
SEE ALSO: Instructions for first aid when bitten by a venomous snake
2. Prepare
Performer : Can be any doctor, nurse, technician or person who has been instructed and practiced.
Means
Bandage: Use elastic bandage 7-10cm wide: 03 rolls. If there is no elastic bandage, it can be used by intravenous tourniquet (be careful not to tour the artery because it causes ischemia, risk of amputation) Splint: Splint for fixation of femur fracture, splint to fix the leg. hand. If not, long sticks, sticks, or large pieces of cardboard can be used. Triangle bandage or forearm sling. Conventional tape: 03 rolls (for fastening the brace). Other tools and facilities: Antiseptic drugs and instruments, washing of bites, respiratory first aid tools (sputum aspiration, ambu ball, intubation, ventilator, oxygen), circulation (intubation set) intravenous lines, fluids, vasopressors), equipment to transport patients (stretchers, ambulances). Patient
Encourage the patient to rest assured, reduce anxiety, do not let the patient walk on their own if the bite is on the leg (because moving the bitten area makes the venom enter the body faster). Take off jewelry (rings, rings) in the bitten area (easy to cause pressure when swollen). Do not try to undress as it can easily move the bitten area, possibly putting a bandage on the garment. Do not let the patient walk on their own. Immobilize the bitten leg or arm (possibly with a splint). Place the bite at or below the heart's level. Explain the need for technique, limit movement of the bitten area. Records, medical records: You can use medical records or a piece of paper to monitor.
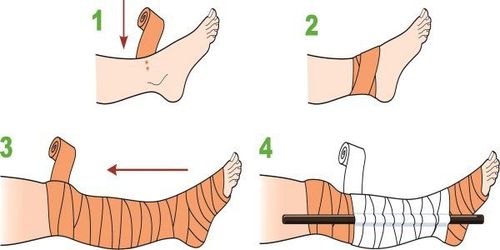
3. Steps to perform the immobilizing bandage technique
Bites on the legs, hands, follow these steps (in order from top to bottom)
Put a bandage on the area around the fingers and feet. The bandage is relatively tight but not excessive (the pulse is still palpable, enough to slip a finger through the folds with difficulty). Start the bandage from your fingers or toes to your groin or armpits (leave your fingernails and toes exposed). Use stiff braces (pieces of wood, sticks, pieces of cardboard, ...) to fix the legs and arms. Bite on table, finger, forearm
Compression bandage, finger, forearm. Use a splint to stabilize the forearm. Use a towel or string to hang around the patient's neck. Bites on the torso, head, face and neck
Use gauze, cloth or folded paper to form a piece about 5cm2 in size, 2-3cm thick, place it directly on the bite and press and hold it continuously on the bitten area but do not limit it. inhibit the patient's chest wall movement or breathing.
Combine other measures on the way to transport the patient to the hospital
If the patient has difficulty breathing: Provide respiratory support according to local conditions, give rescue breaths, squeeze ambu balloon through a mask or then intubate Squeeze ball or mechanical ventilation.
When to remove the compression bandage
Maintain the compression bandage until the patient reaches a medical facility capable of emergency resuscitation (can be intubated with balloons or mechanical ventilation).
Preparation before removing the compression bandage:
Place an intravenous line. Drugs: 0.9% sodium chloride solution or Ringer lactate intravenous infusion to maintain the line and anaphylaxis. Respiratory emergency equipment: Oxygen, ambu balloon, intubation kit, ventilator. How to remove the tape: Remove slowly, slowly remove each part.
Closely monitor the patient's pulse, blood pressure, skin color, respiration and paralysis during and after removal.
4. Follow up
Monitor vital signs: Sensation, pulse, blood pressure, breathing rate. Paralysis of the patient: Patients paralyzed by a cobra bite often have paralysis in the anterior cranial nerves (throat pain, drooping eyelids, blurred vision, difficulty speaking, difficulty swallowing), then paralysis of the intercostal muscles, muscles diaphragm and eventually paralysis of the limbs. The feeling of pain, tension, and numbness in the bitten limb is covered with a bandage. The skin color of the tips of the fingers and nails of the limbs are bandaged. Posture, position and movement of the bitten area Tightness of the bandage.
5. Handling complications
The immobilization technique is assessed as safe. However, there is often a tendency for the compression band to not be tight enough, resulting in limited effectiveness.
Compression causes distal ischemia:
Uncommon if done correctly, usually because the bandage is too tight, lasts for many hours and swelling progresses. Manifestations: Pain, numbness, loss of sensation in toes, fingers, color of toes, toenails, purple nails. Treatment: Loosen the bandage but still ensure the pressure. With areas near Vinmec Health System hospitals that can immediately transfer patients to Vinmec hospital, the hospital always prepares adequate human resources to deal with food poisoning cases, preventing further poisoning. .
Vinmec International Hospital's Emergency Resuscitation Department operates 24/24 on all days of the week, including Saturdays and Sundays as well as holidays of the year. With diagnostic imaging equipment and Modern testing, especially specialized heavy-duty ambulances with a full range of supporting machines for severe patients traveling long distances in the subclinical field as well as in transporting serious patients on request. . The team of emergency doctors and nurses at the Emergency - Resuscitation Department of Vinmec International General Hospital are intensively and professionally trained, able to receive and handle urgent cases of patients, and at the same time always has coordinated with all specialties of the Hospital in a methodical and quick manner. At Vinmec Emergency and Resuscitation Department, patients will be examined, diagnosed, quickly and accurately treated and treated according to the priority of emergency until the critical condition is over.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.