This is an automatically translated article.
Article by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital.
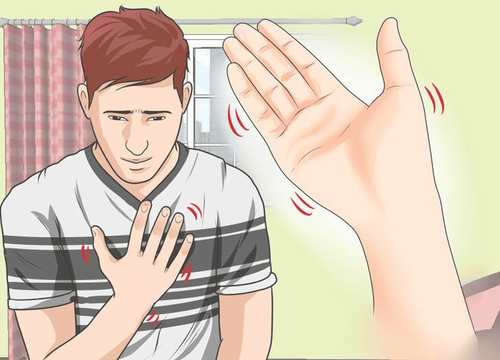
Fibromyalgia is a disorder that causes pain in the muscles and bones, causes fatigue, and can affect sleep and mood. Fibromyalgia complications affect lifestyle, depression, and more.
1. Causes of fibromyalgia
The exact cause of fibromyalgia is still unclear, but some possible causes include:
Genetics Infections Physical or emotional trauma Some researchers are investigating how the system The central nervous system (CNS) processes pain and how it may increase pain in people with fibromyalgia, possibly due to an imbalance of neurotransmitters in the brain.
Fibromyalgia symptoms may come and go. Pain syndrome can disrupt life and make daily activities more difficult. However, people living with fibromyalgia can manage their symptoms by:
Coping with pain using available treatments Avoiding flare-ups Manage tight complications
2. Effects of fibromyalgia
Symptoms like joint pain can limit your mobility and make it harder for you to concentrate on everyday activities like working.
Fibro fog (Brain fog syndrome) is also a major symptom for fibromyalgia patients. This is a serious condition that can lead to impaired functioning both physically and mentally. Fibro fog is a cognitive dysfunction characterized by:
Easily distracted Difficulty talking Short-term memory loss Forgetfulness Because of these symptoms, many people with fibromyalgia are unable to function. For people who are able to work, fibromyalgia can still reduce productivity and possibly reduce their quality of life. It can make things that were once enjoyable difficult because of the pain and fatigue that come with the condition.
The pain of fibromyalgia can limit your ability to function and can cause you to withdraw from your usual activities and social life. Fibromyalgia flares up due to stress and can also be caused by depression and isolation. A cycle of pain and isolation can ensue.

3. Diseases associated with fibromyalgia
Many health problems are more common when you live with fibromyalgia. However, being aware of these associated diseases can help you identify symptoms and differentiate between fibromyalgia and another underlying disorder.
The following related conditions are more common in people with fibromyalgia :
Chronic fatigue syndrome Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) Migraines Tension headaches Late endometriosis (a female reproductive disorder) Lupus (an autoimmune disease) Osteoarthritis Rheumatoid arthritis (RA) Restless legs syndrome Many of these conditions can be easily identified Okay. The doctor can prescribe specific treatments for the patient.
Other symptoms such as intestinal disease can present a more difficult challenge. However, it is reported that up to 70% of people with fibromyalgia have the following symptoms:
Diarrhea Constipation Abdominal pain Bloating These symptoms are a sign of IBS. Fibromyalgia may also be present in patients with IBD, such as Crohn's (CD) and ulcerative colitis (UC).
The 1999 study published in the Journal of Rheumatology involved 113 patients with IBD, namely 41 Crohn's patients and 72 ulcerative colitis patients.
Research shows that 30% (30 patients) have fibromyalgia. Nearly 50% of patients with Crohn's disease have fibromyalgia, while about 20% of patients with ulcerative colitis have it. The researchers concluded that fibromyalgia is common in people living with IBD.
Distinguishing between fibromyalgia and related conditions can help you identify and treat the condition causing your symptoms.
Some activities that can help treat fibromyalgia pain and improve your overall health include:
Reduce stress Get enough sleep Try to eat a healthy diet Exercise regularly moderate exercise
4. Fibromyalgia and depression
Many people with fibromyalgia also experience depression. Some people believe that depression and fibromyalgia have some biological and psychological similarities. If so, this means that one disease may be accompanied by another. About 90% of people with fibromyalgia have depressive symptoms. The isolation and pain that often accompanies this disorder can lead to depression.
In addition, some health care providers still believe that the syndrome is not an actual disease. They believe it's a combination of several symptoms caused by stress, and that it's "all in one's head," which can also lead to depression.
Therapy can help you deal with depression. In-person sessions can help you understand what's going on with your body and how your thoughts can affect your health. Support groups also benefit. They can help you identify with others who have a medical condition and help alleviate feelings of loneliness or isolation.

5. Fibromyalgia Treatment
Currently, there is no known cure for fibromyalgia. However, treatments are available to help you manage pain and flare-ups. In some cases, treatment can provide gradual pain relief.
Treatment may include:
Pain medication, used with caution because of potential addiction Physical therapy Exercise, preferably aerobic Cognitive behavioral therapy (CBT) Alternative medicine such as acupuncture, meditation and tai chi If you are experiencing symptoms of a related illness, it is important to see your doctor for a thorough evaluation for:
Identify differences in symptoms Confirmation of diagnosis Proper treatment of fibromyalgia and any underlying condition Most people with fibromyalgia find their improvement most when they are able to create and maintain a good symptom management plan. This may include a combination of medication and alternative treatments, or therapy to help the person cope with the psychological effects of the disorder.
No matter what symptoms you have or how severe your condition is, there are treatment options that can help you live a healthy and fulfilling life. Talk to your doctor about creating a treatment plan that's best for you.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Buskila D, et al. (1999). fibromyalgia in inflammatory bowel disease. ncbi.nlm.nih.gov/pubmed/10332985 Fibromyalgia. (n.d.). fibroandpain.org/what-is-fibromyalgia-2 Chang L. (n.d.). The association of irritable bowel syndrome and fibromyalgia. med.unc.edu/ibs/files/2017/10/fibromyalgia -and-IBS.pdf Fibromyalgia. (2014). niams.nih.gov/health-topics/fibromyalgia Gracely RH, et al. (2012). fibromyalgia and depression. DOI: 10.1155/2012/486590