This is an automatically translated article.
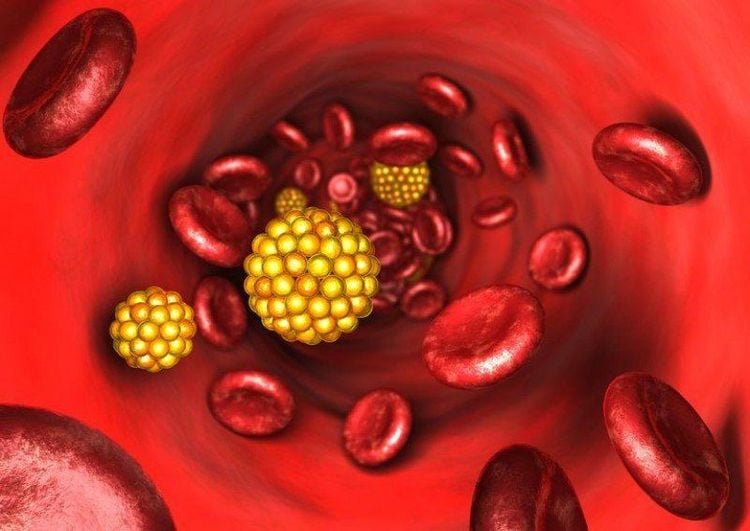
Familial hypertriglyceridemia (familial dyslipidemia type IV) is a disorder characterized by overproduction of very low-density lipoproteins (VLDL) from the liver. As a result, the patient will have an excessive amount of triglycerides and VLDL, which can cause acute pancreatitis. This article addresses the assessment and treatment of familial hypertriglyceridemia and highlights the role of interdisciplinary collaboration in the assessment and treatment of this condition.1. What is familial hypertriglyceridemia?
Familial hypertriglyceridemia (familial dyslipidemia type IV) is a disorder characterized by overproduction of very low-density lipoproteins (VLDL) from the liver. As a result, the patient will have too much triglycerides and VLDL in total body lipids.This disorder usually occurs due to autosomal dominant inheritance. Clinically, familial hypertriglyceridemia presents in patients with mild to moderate laboratory elevations in triglyceride concentrations. Familial hypertriglyceridemia is often accompanied by other comorbidities such as obesity, hyperglycemia, and hypertension.
Patients with this disorder are usually heterozygous for mutations that inactivate the lipoprotein lipase (LPL) gene. Although this mutation alone can significantly increase triglycerides in the body, the combination of other drugs or comorbidities can aggravate the elevation of serum triglycerides to the point of disease. physical. A significant increase in triglycerides can lead to some clinical manifestations of dyslipidemia and acute pancreatitis.
When discussing familial hypertriglyceridemia is divided into categories according to Fredrickson-Levy and Lee (FLL). Includes types I, IIa, IIb, III, IV, and V. Familial type IV dyslipidemia is considered familial hypertriglyceridemia and can be differentiated from other types based on lipid testing. of the patient.
The frequency of heterozygous carriers of different pathological mutations in the LPL gene ranges from 0.06% to 20% (note that different mutations exhibit different degrees of pathology) .
2. Causes of familial hypertriglyceridemia:
While familial hypertriglyceridemia is often associated with autosomal dominant inheritance, it should be noted that most cases are polygenic, separating the disorder from Mendelian inheritance. classic.
A common mutation associated with the development of familial hypertriglyceridemia is a heterozygous inactivation mutation of the LPL gene. The inactivation of this gene enables the body to hydrolyze the triglycerides in the VLDL core. This creates an accumulation of triglycerides and VLDL, which contributes to pathology.
The second cause is insulin. Insulin is also a potent activator of LPL in adipose tissue. Thus, insulin resistance may decrease LPL activity and ultimately contribute more to hypertriglyceridemia, causing blood triglyceride levels to rise to pathological levels.
In addition to the classical understanding, hypertriglyceridemia may be directly related to a number of different loci in the gene allowing for additional pathological changes, besides hypertriglyceridemia, some components may be disturbed. other lipids.
Có nhiều nguyên nhân có thể gây tình trạng tăng triglycerid máu
3. Symptoms of familial hypertriglyceridemia:
A patient with familial hypertriglyceridemia usually has no symptoms unless the disease is advanced. Some factors that trigger this condition are: stress, psychological trauma. In some special cases, the disease will manifest from the very beginning.
In hereditary dyslipidemia, patients may present with variants of cutaneous xanthomas. Jaundice is essentially a collection of “lipid-filled” macrophages. These macrophages accumulated too much free lipids and became “foam cells”. Yellow tumor is often seen on eyelids, elbows, knees,... with a size less than 5mm. If you find yellow lumps on the skin, it is a sign of hypertriglyceridemia. However, it should be noted that the triglyceride concentration in the presence of these lesions is significantly higher than that in the blood of patients with familial hypertriglyceridemia.
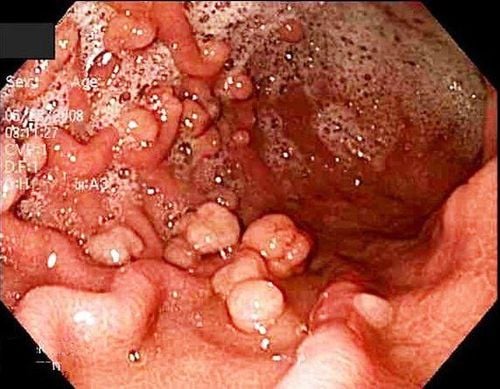
The second manifestation which is also a complication of familial hypertriglyceridemia is acute pancreatitis. Pancreatitis results from the conversion of pancreatic exocrine pro-enzymes to the “active” form within the pancreas, which causes the digestion of the pancreatic tissue itself and causes acute pancreatitis.
4. Grading of familial hypertriglyceridemia:
This classification is based on the determination of the patient's fasting blood triglycerides. According to the Endocrine Society cited by Berguland et al., this pathology is classified into degrees:
Mild: 150 to 199 mg/dL Moderate: 200 to 999 mg/dL Severe: 1000 to 1999 mg/dL Very severe: ≥2000 mg/dL Evaluation of hypertriglyceridemia should not stop with lipid testing. Physicians must check regularly and monitor the progress of other comorbidities that may aggravate the condition.

Người bệnh tăng triglycerid máu cần được thăm khám định kì
5. Treatment of familial hypertriglyceridemia:
Treatments for familial hypertriglyceridemia focus on lowering triglyceride levels. Furthermore, if the patient has pathologically elevated triglyceride levels, treatment of the other cause of the hypertriglyceridemia will be important to maintain a relatively normal lipid level.
Current recommendations recommend routine monitoring of mild to moderate hypertriglyceridemia to assess cardiovascular disease risk. In addition, severe hypertriglyceridemia should be evaluated for possible development of pancreatitis. Finally, initial treatment of severe hypertriglyceridemia alone should be initiated with fibrate therapy.
Specific treatments used to control hypertriglyceridemia include fibrates as first-line drugs. Drugs such as fenofibrate and gemfibrozil help activate LPL through PPAR-alpha, leading to further breakdown of triglycerides. Fibrates have been shown to markedly reduce triglyceride levels by 50% or more, due to their effectiveness and place in the treatment protocol.
The combination of fibrate and statin may worsen side effects caused by statins. This is hypothesized to be due to inhibition of CYP-3A4 via fibrates. If combination therapy is required, use caution and consider statin therapy not primarily metabolized by CYP-3A4 (pravastatin).
Nicotinic acid (niacin) is commonly used as an adjunct to therapy. Niacin adjuvant is most useful in patients not treated with fibrate monotherapy and who are at high risk for pancreatitis.
Another useful supplement for better reinforcement treatment is fish oil. Fish oil has been shown to significantly reduce both VLDL and triglyceride levels.
New developments in the genetics of hypertriglyceridemia are showing great promise for further predicting cardiovascular risk. Accurate prediction will allow earlier treatment for better disease progression. Furthermore, genetic development is currently being studied and found ways to repair genes.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference article: pubmed.ncbi.nlm.nih.gov