This is an automatically translated article.
The article was professionally consulted by Doctor Do Thi Hoang Ha - Doctor of Biochemistry - Laboratory Department - Vinmec Hai Phong International General HospitalIf your doctor tells you that you have porphyria, it means you have a disorder that can cause problems with your nerves, skin, and urinary system. While there is no cure, the following insights can help you manage your symptoms and lead a normal life like those around you.
1. What is porphyria?
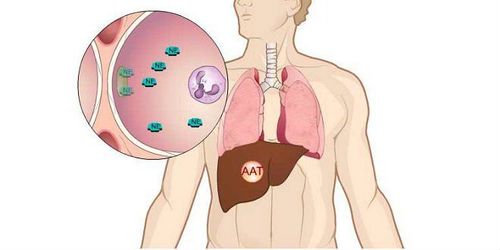
Porphyrias are the result of an inherited or acquired enzyme deficiency in the heme biosynthetic pathway, which affects how the body synthesizes it. These deficiencies result in accumulation of toxic heme precursors. Heme is an iron-containing protein, which gives blood its red color, and is an essential cofactor of many hemoproteins. Almost all cells of the human body need and synthesize heme, which helps the blood carry oxygen to every cell in the body. However, most of the heme is synthesized in the bone marrow (by red and white blood cells) and incorporated into hemoglobin. The liver is the second most active site for heme synthesis, most of which is conjugated with cytochrome P-45 enzymes.Heme synthesis requires 8 enzymes, which create and transform special molecules called porphyrins (and their precursors); The accumulation of these substances causes the clinical manifestations of porphyrias. There are about 8 different types of porphyrias. Most of these are due to abnormalities in genes that are passed down through generations. In addition, genetic material can also be damaged by exposure to certain chemicals, alcohol, or liver infections. Two major clinical manifestations of this disease occur: sympathetic nervous system abnormalities (acute porphyrias) and photosensitivity skin (cutaneous porphyrias).

2. Causes of porphyria
Porphyrias are identified by a lack of certain enzymes and result from a deficiency in any of the last 7 enzymes of the heme synthesis pathway or from increased activity of the first enzyme in the pathway, ALA synthase- 2 (ALAS 2). When an enzyme that synthesizes heme is missing or defective, the heme is easily destroyed, its substrates and other heme precursors modified by that enzyme can accumulate in the bone marrow, liver, skin, or other tissues and is toxic. These precursors may appear in excess in the blood and be excreted in the bile, faeces, or urine, causing porphyria.The cause of most types of porphyrias is genetic. That means when one or both of your parents pass the mutated gene to you, you'll get the condition. Autosomal dominant inheritance (AD) is the most common, in addition there are many different types of mutations (autosomal recessive or X-linked inheritance).
In addition to genetic factors, there are other triggers that suddenly affect heme synthesis that can also cause porphyria such as:
Drinking a lot of alcohol; Women using estrogen; Liver diseases (Hepatitis C, cirrhosis); HIV ; Smoke; Sun exposure; Use of drugs: Barbiturates, some antibiotic families, oral contraceptives; Severe toxic infection.

3. Symptoms of porphyria and porphyrinuria
Symptoms of an acute porphyria can appear and progress rapidly over days or weeks and can be very severe, manifesting in episodes, often stimulated by medication, and cyclic hormonal activity. in young women and other exogenous factors. Symptoms may include:Abdominal pain, often of severe severity, with intermittent episodes of unknown cause; Chest pain, difficulty breathing; Tachycardia and increased blood pressure; Back pain, muscle weakness and cramps; may lead to paralysis Skin loss of sensation; Nausea, vomiting and constipation ; convulsions; Neuropsychiatric disorders: The person has personality changes, is prone to depression or other mental disorders (anxiety, confusion, hallucinations, disorientation or paranoia). At times, the person may feel agitated, confused, or have a seizure. In addition to acute attacks of porphyria, another form of porphyria is cutaneous porphyria. In which, the most prominent symptoms are lesions on the skin, which are very sensitive to light, easily damaged, with water cysts, and water burns. The most commonly affected areas are the back of the arms, forearms, behind the ears, neck, hair growth, excessive hair in the affected areas. These skin lesions are very susceptible to infection leading to cellulitis, sepsis. As the skin heals it may have an irregular appearance of color, thin easily, or leave a scar.
Simultaneously with the above manifestations is the phenomenon of porphyrinuria. Patients are easily alarmed with sudden episodes of dark urine, especially when out in the sun. Urine is dark yellow or turns sassafras-colored, centrifuged without red blood cells settling at the bottom. It is the heme cores that are destroyed and eliminated.

Acute episodes of porphyrias can still be life-threatening if not treated promptly. During an acute attack, the amount of heme is massively destroyed in the blood, causing the patient to lose water, have difficulty breathing, urinate, convulsions and very high blood pressure. Long-term complications of recurrent acute attacks with high frequency may include persistent systemic pain, chronic renal failure, and permanent liver damage; Skin porphyrias can lead to permanent skin damage. In addition, the blisters on the skin can become infected. When the skin lesion heals, it may still have an irregular shape and color, break easily, or leave a bad scar.
4. How is porphyria diagnosed?
Although the full-blown symptoms are quite intense, doctors sometimes have trouble making an early diagnosis because the first symptoms can be similar to other illnesses. At this time, the indications for blood tests, the determination of porphyrins in urine and feces for diagnosis are extremely necessary. The best time to have these tests is as soon as a person has a flare-up of the symptoms listed above. Asymptomatic patients, including suspected carriers and those in between exacerbations, were similarly evaluated. However, these tests are less sensitive in these cases; RBC or WBC enzyme activity measurements are considered to be more sensitive.The doctor may also recommend genetic testing, not only for the patient himself but also for other family members. Genetic analysis is very accurate and preferred for use in families when mutations are identified. Prenatal testing (amniocentesis or chorionic villus sampling) is possible but is rarely indicated.
5. How to treat porphyria

If you have a chronic porphyria, treatment will depend on the specific type of disease you have and the severity of your symptoms. In particular, the basic treatment regimen will include:
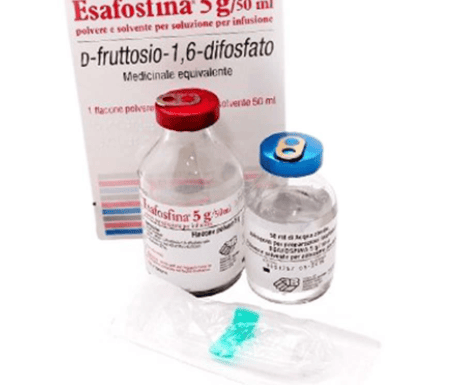
Regular blood extraction, ie removing a part of the blood and replacing it with an electrolyte solution of the same volume to reduce the amount of iron stagnation in the liver and other internal organs. other organs; especially with cutaneous porphyria. Indication of low doses of the antimalarial drugs chloroquine or hydroxychloroquine; should only be used in those who cannot tolerate blood extraction. Inject hemin, a drug that looks like heme, to limit the body's production of Porphyrin. It is recommended to avoid factors that can cause porphyria, such as psychological stress, alcohol consumption, smoking, sun exposure, etc. Before taking any medication, consult your doctor. . Avoid taking birth control pills. Enhance natural resistance to limit infection; People with porphyrins should receive genetic counseling before marriage and pregnancy. In a nutshell, porphyria are a group of disorders of heme metabolism in the body. Genetic diseases are chronic. Although there is no radical treatment, if the disease is detected early and actively avoids the factors that trigger the occurrence of porphyria, the patient can still lead a life assimilated into the community like normal people.
If you have any suspicious signs of porphyria or have a family member with the disease, you should soon seek out reputable medical facilities for examination and testing and combination. with other diagnostic methods. Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading doctors, modern equipment and technology, but also stands out for its examination and consulting services. and comprehensive, professional medical treatment; civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: webmd.com; .mayoclinic.org