This is an automatically translated article.
Written by Doctor Luong Vo Quang Dang - Cardiologist - Head of Internal Medicine Department - Department of Medical Examination & Internal Medicine, Vinmec Phu Quoc International HospitalExercise-induced bronchospasm (EIB) is defined as a temporary narrowing of the small airways that occurs after strenuous exercise. EIB can occur in asthmatic or non-asthmatic patients based on spirometry.
1. Overview of exercise-induced bronchospasm
The concept of Exercise Induced Asthma has been known for a long time, even before BC, that exercise can cause asthma symptoms in some patients. However, this concept only became popular and interested in the 60s and 70s of the last century, when there were reports explaining the mechanism of airway response to exercise and the effects of drugs. exercise-induced asthma.It was not until 2010 that a panel of experts met and agreed for the first time to coin the term Exercise Induced Bronchoconstriction (EIB) instead of exercise-induced asthma, because it is actually Exercise (or exertion) does not cause asthma, but only bronchospasm.
Currently, Vinmec Phu Quoc International General Hospital has implemented methods to help diagnose exercise-induced bronchospasm, to help patients with this condition be properly diagnosed and treated appropriately. reduce the risk and impact of the disease. The following article will help us better understand this medical condition, prevention and appropriate treatment.

2. What is exercise-induced bronchospasm?
Exercise-induced bronchospasm (EIB) is defined as a temporary narrowing of the small airways that occurs after strenuous exercise. EIB can occur in asthmatic or non-asthmatic patients based on spirometry. If associated with asthma, EIB is an indication for initiating regular controller medication and also an indicator of inadequate asthma control.
To date, the most recent definition of EIB is an acute (temporary and reversible) airway narrowing that occurs after strenuous exercise. EIB can occur during or after strenuous exercise
3. How common is EIB?
The frequency of EIB in the general population ranges from 5 to 20% . In children, the rate is between 3.1 and 16.0%. In asthmatic patients, the frequency of EIB can be as high as 90%. In particular, the rate of EIB is higher in patients with severe asthma or poorly controlled asthma.) In professional athletes, EIB rates range from 30 to 70 percent, depending on the sport, environmental conditions and maximum intensity of that sport.
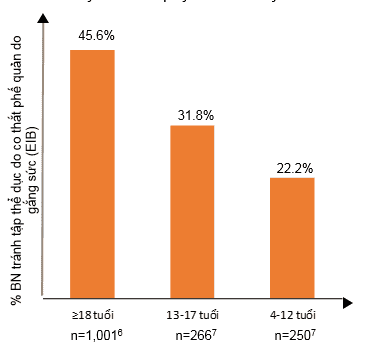
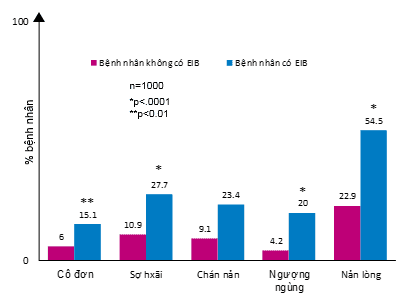
Regular physical activity improves the prognosis of asthma, but EIB causes asthma patients both adults and children to limit exercise, especially in adults by nearly 50%. (chart 1-A). Not only restricting physical activity, EIB also adversely affects patients' emotions (chart 1-B). EIB can present with symptoms ranging from mild, limited physical activity, to severe bronchospasm leading to respiratory failure and even death.
4. Pathogenesis of EIB
When the patient is active, it will lead to hyperventilation, if the air is dry, it will lead to dehydration of the airway epithelial surface by evaporation. And at this time 2 mechanisms are activated: osmotic mechanism and thermal mechanism.
Osmosis mechanism: dehydration of the mucosa leads to cell atrophy, creating a hypertonic environment by increasing the concentration of intracellular Na+, Cl-, K+ ions, when cells are contracted. causes the release of chemical mediators that cause bronchospasm, edema, and increased vascular permeability, thereby causing EIB.
Thermal mechanism: after evaporation on the surface causes cold on the mucosal surface causing vasoconstriction. The airways then warm again and increase vascular permeability and cause edema, which in turn causes EIB.

5. What are the symptoms of EIB and how is it diagnosed?
Regarding the diagnosis of EIB at present, there are many difficulties such as non-specific, vague symptoms, symptoms that are usually considered normal manifestations of physical exertion, questionnaires often cannot diagnose Diagnosis based on symptoms and signs alone, athletes are often stubborn, diagnoses based solely on symptoms reported by patients are often unreliable.By far the most commonly used flowchart in the diagnosis of exercise-induced bronchospasm

6. How to prevent and treat EIB?
Once the diagnosis of EIB has been confirmed, treatment will include 3 main goals:
Preventing symptom onset during exercise Improve symptoms when it has already occurred Improve overall asthma control (if any) ) To achieve the above treatment goals, there are 2 non-pharmacological and pharmacological therapies.
First, about non-drug therapy:
Warm up well before exercise (experts recommend warming up to reach 60-80% of maximum heart rate) After exercise, gradually cool down Reduce or avoid triggers and exposure Use a mask in cold weather Avoid exercise in cold and dry air Breathe through your nose In terms of drug therapy, there are 5 main groups of drugs including:
Stimulant drugs β2 :
Use short-acting β2 agonists (SABAs) by inhalation to prevent EIB and accelerate recovery of lung function after exercise-induced impairment. (Strong recommendation; Evidence A) Intermittent (<4 times/week) use of SABA, LABA monotherapy, or both prior to exercise as these agents may prevent or mitigate EIB. (Strong recommendation; Evidence A) Caution is advised in the daily use of β2-agonists, alone or in combination with ICS, because this may lead to decreased response, through a reduction in duration. effects, reduced effectiveness, or both in preventing EIB and prolonging recovery time with post-exercise SABA use. (Strong recommendation; Evidence A) Leukotriene receptor antagonists (LTRA):
Daily use of leukotriene receptor antagonists may be considered because they do not lead to tolerance and have been shown to reduce EIB in about 50% of patients. This medicine can also be used intermittently or continuously for prevention. However, it does not completely prevent or be effective in reversing airway obstruction. (Strong recommendation; Evidence A) Mast cell stabilizers:
Consider inhaled cromolyn sodium and nedocromil sodium just before exercise. This slightly reduces EIB but may have short-term effects. This group of drugs does not have a bronchodilator effect. They can be effective when used alone or in combination with other drugs. (Strong recommendation; Evidence A) Inhaled/inhaled corticosteroids (ICS):
Consider ICS in combination with other agents because ICS may reduce the frequency and severity of EIB but not the severity of EIB. Complete eradication of EIB (Strong Recommendation; Evidence A) Do not use daily ICS/LABA to treat EIB unless necessary to control moderate to severe asthma. ICS may not prevent resistance to β2-agonists from daily use. (Strong recommendation; Evidence A) Anticholinergics:
Consider ipratropium bromide for patients unresponsive to other classes of drugs; however, its EIB reduction effect is not uniform. (Weak recommendation; Evidence A)
7. Conclusion
EIB is very common in athletes and asthmatics, but is still largely underdiagnosed. Clinicians should distinguish between two groups of patients, those with EIB alone or those with persistent asthma and exercise as an asthma trigger. Non-drug measures such as warm-up carefully, avoiding allergens and cold air, wearing a mask, and short exercise time should be applied to all patients. SABA and LTRA are effective in preventing bronchospasm. And patients with persistent asthma should receive long-term maintenance ICS. Future research is needed to find a means of distinguishing EIB from other forms of exercise-related dyspnea, such as screening questionnaires. The concept of EIB phenotype is also a good suggestion for future researchers.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.