This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
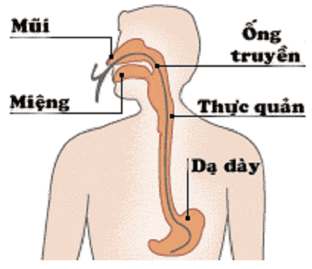
1. Methods of feeding through the tube
Parenteral nutrition is a common feeding method in critically ill patients in hospitals in cases such as anorexia, severe malnutrition where the patient cannot eat normally through the mouth.
This method includes techniques
Percutaneous gastrostomy tube feeding
2. Enteral nutrition support through feeding tubes- When to consider
There are very few published reports on the use of home enteral nutritional support (enteral nutrition) in short bowel syndrome. In a recent report from a large at-home enteral nutrition program in Canada, only 9 of 727 patients received home parenteral nutrition for short bowel syndrome. Despite its apparent use in adults with short bowel syndrome, in short bowel syndrome patients unable to meet their nutritional and/or fluid needs by mouth, a clinical trial of nutrition Intestinal tract should be considered to prevent the need for a central venous catheter and support intravenous nutrition.
This intervention may be most successful in patients with some remaining colon, while its use in patients with a terminal jejunostomy may increase anal fecal output causing obstruction. Sleep and quality of life are further impaired. If enteral nutrition is to be pursued, we recommend a trial of the nasogastric tube before considering a more permanent percutaneous approach.
In patients whose diet and medication are optimized, it will soon become clear whether this plan is successful based on changes in stool loss. Formula should be inserted into the stomach via a continuous infusion to slow down the nutrient delivery to maximize nutrients: time of contact with the mucosa, thus, optimizing simultaneous absorption reduce diarrhea.
Overnight infusion takes advantage of the gastrointestinal tract when nothing else competes with the mucosal receptors for absorption; Plus, it doesn't interfere with daytime activities. The use of a standard lower osmolarity polymer formulation containing a mixture of LCT and MCT maintains mucosal structure and function and enhances intestinal adaptability; Supplementation of fiber as part of an enteral product or as a soluble fiber supplement is recommended in patients with small bowel remaining.
In addition to not outperforming standard macromolecular products, the hyperosmolar properties of elemental products can actually increase the amount of manure. Finally, because appropriate bile salt supplements are not available, patients with bile salt deficiency will benefit from a lower fat formulation.

3. Parenteral nutrition
Almost all patients with short bowel syndrome require parenteral nutrition support (intravenous nutrition) in the early period after surgical resection, and most will require nutritional support. parenteral care at home after they leave the hospital. The caloric requirement of parenteral nutrition will depend on many factors such as weight gain (or loss), exercise/activity level... and there is no one-size-fits-all prescription.
Parenteral nutrition should be initiated and adjusted to meet the patient's fluid, electrolyte, energy, protein, and micronutrient needs. The overall energy content and macronutrient composition will depend to some extent on the intake of the short bowel syndrome patient and the level of supplementation required. In situations of high rectal output, increased fluid volume, loss of potassium, magnesium, and zinc will occur and should be monitored and appropriately replaced. The amount of parenteral nutrition may be reduced when the patient demonstrates the ability to absorb oral nutrition without excessive fecal or rectal discharge with appropriate weight gain or maintenance. When calculating the volume and content of parenteral nutrition, changes in the patient's weight, laboratory tests, stool or anal volume, urine output, and complaints of thirst should be considered. These patients are still at risk of micronutrient deficiencies and require periodic monitoring and supplementation in addition to parenteral nutrition.
Home parenteral nutrition is usually given overnight for 10 to 14 hours so that patients do not need to be pumped during the day and potentially reduces the risk of liver damage with long-term use. In some patients, the volume needed can cause high volume nocturia. These patients may do better with less fluid at night and one or two liters of intravenous “chaser” in the morning or evening before they have their parenteral nutrition added at night. .
Programmable infusion pumps are used by most consumers. Portable pumps that can be carried in a backpack or tote are also available for parenteral nutrition consumers who have day-to-day infusion needs. Patient support groups such as the Oley Foundation (www.oley.org) are an important source of information on practical topics (e.g., body image, travel), education, support, and possibly reduce the risk of complications, and improve the survival and quality of life of patients receiving enteral or parenteral nutrition support.

Programmable infusion pumps are used by most consumers. Portable pumps that can be carried in a backpack or tote are also available for parenteral nutrition consumers who have day-to-day infusion needs. Patient support groups such as the Oley Foundation (www.oley.org) are an important source of information on practical topics (e.g., body image, travel), education, support, and possibly reduce the risk of complications, and improve the survival and quality of life of patients receiving enteral or parenteral nutrition support.
CONCLUSION
Nutrition therapy is central to the successful management of patients with short bowel syndrome. Continuing and important education to the extent that the patient/carer can be understood from the outset is essential and sufficient time must be devoted to this purpose. As the gut adapts and improves absorption, it is possible that dietary interventions could be released. Lifelong follow-up is necessary in all patients with short bowel syndrome, and management goals often change over time.
Currently, Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic techniques for digestive diseases, short bowel syndrome, chronic diarrhea, Crohn's disease , gastric mucosa is displaced in the esophagus...
Vinmec Hospital with modern facilities and equipment and a team of experienced experts, always dedicated to medical examination and treatment, customers can You can rest assured with gastroscopy and esophagoscopy service at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














