This is an automatically translated article.
Articles written by MSc, BS. Bui Chi Nam, Department of General Internal Medicine, Vinmec Times City International General Hospital
Endoscopic retrograde cholangiopancreatography is a safe, minimally invasive procedure to help diagnose and treat a number of biliary and pancreatic diseases. So how is this technique performed, does it cause complications?
1. What is ERCP?
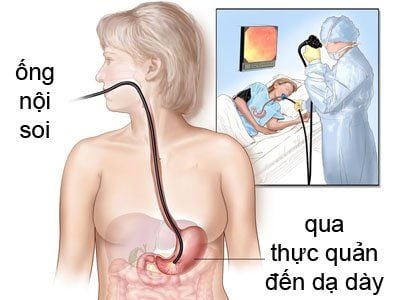
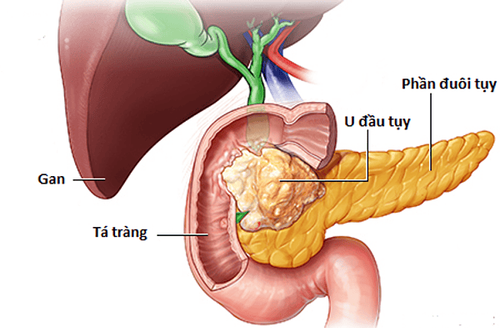
Endoscopic Retrograde Cholangio - Pancreatography (ERCP) is a technique that uses an endoscopic lateral view (endoscope) to endoscopy by mouth through the stomach into the second part of the duodenum. to the place where bile and pancreatic juice are poured into the intestine (Papilla's knob) to enter the biliary tract, the pancreas to diagnose and treat some diseases of the bile ducts and pancreas such as common bile duct stones, pick up worms in the bile ducts, place stents drainage in case of biliary obstruction due to tumor etc..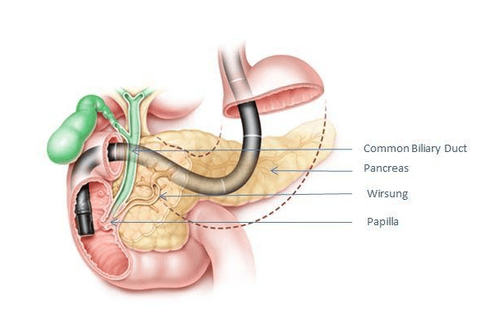
Hình 1. Hình ảnh minh họa kỹ thuật ERCP: Máy nội soi (màu đen); Nhú tá tràng (Papilla); Ống tụy chính (Wirsung); Ống mật chủ (Common Biliary Duct); Tụy (Pancreas).
2. What are the applications of ERCP?
2.1 Diagnostic ERCP Cholangiography, pancreas: Diagnosing biliary and pancreatic diseases such as biliary strictures, pancreas, gallstones, etc.. biopsy by pliers or brush specimens to diagnose cholangiocarcinoma, pancreas. Endoscopic cholangiopancreatography (Spy Glass DS): Is an endoscope to directly observe the biliary tract, diagnose diseases: Diagnosis, biopsy specimens to confirm diagnosis of cholangiocarcinoma, gallstones etc.. 2.2 ERCP treatment Sphincterotomy: Treatment of stenosis or loss of muscle function of Oddi (sphincter of Oddi dysfunction); Disperse and remove common bile duct stones; Get worms in the bile ducts; Acute pancreatitis due to obstruction of Oddi stones; Cholestasis with dilatation of the common bile duct, pancreatic duct of unknown cause; Pancreatic head tumor, cholangiocarcinoma (relative indication); Treatment of bile leaks after surgery; Drainage of pancreatic pseudocyst; Placement of stents to drain the biliary tract to prevent biliary and pancreatic obstruction.3. How is ERCP performed?
ERCP is performed by a gastroenterologist or surgeon who has specialized training in this technique. The scope is a long, flexible tube with a light and camera on the end. Patients are pre-anesthetic or general anesthesia, so during the procedure, the patient will not feel any discomfort or pain, the patient will be examined and consulted by an anesthesiologist before the procedure. This technique is performed in a procedure room with all necessary equipment such as: Side window endoscope, vital function monitor, ventilator and C-ARM X-ray machine, etc... The patient lies on the left side or prone on the procedure table, the scope is inserted into the mouth, through the esophagus, stomach, and then to the place where the bile duct enters the duodenum (papilla). A plastic catheter (Cathete) is inserted into the bronchoscope to reach the tip of the tube and then inserted into the duodenal papilla up the biliary tree. Next, the doctor will inject contrast material into the bile ducts and conduct X-rays to clearly show the biliary tract, pancreas and pathologies such as gallstones, biliary strictures due to tumors, etc... By By examining the bile ducts in this way, obstructions, gallstones, tumors, or duct abnormalities can all be detected. If abnormalities are found, the doctor can perform techniques to treat or improve the condition. For example, if a stone is found, the doctor may dilate or cut the muscle of Oddi with an electric knife and then dissolve and remove the stone from the common bile duct or may place a stent to drain the bile to prevent biliary obstruction and improve urinary tract infection. secret etc...
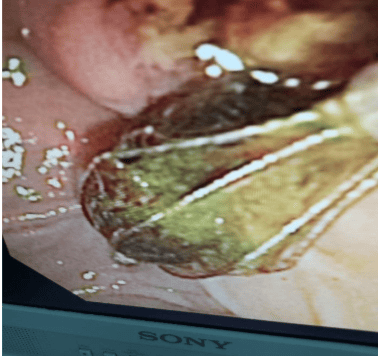
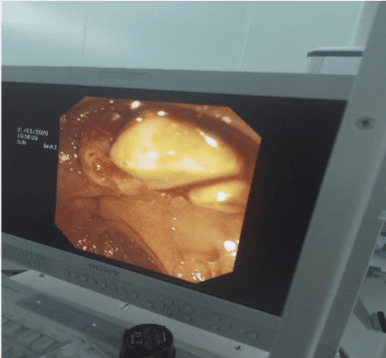
Hình 2. Ứng dụng ERCP lấy sỏi mật, tụy tại Bệnh viện Đa khoa Quốc tế Vinmec Times City
4. What does the patient need to prepare for the ERCP?
Before ERCP intervention, the patient must be fasted before 6 -8 hours or longer to ensure that the stomach is no longer empty, to avoid fluid and food reflux into the lungs during ERCP. Most medications can be taken prior to ERCP. Certain medications need to be adjusted prior to endoscopy, e.g. antidiabetic drugs, anticoagulants or antiplatelet agents that need to be weighed against risk factors for procedural bleeding or thromboembolism during the procedure. stop the drug. In general, aspirin and anti-inflammatory analgesics can be safely used during ERCP. Prophylactic antibiotics are necessary, and should be given 2 h before ERCP intervention. Tests before conducting ERCP: + Chest X-ray, abdominal ultrasound, electrocardiogram, gastroscopy, magnetic resonance imaging (MRI) of the biliary tree.
+ Tests recommended before laparoscopy: Beta HCG test in women of childbearing age.
+ Basic coagulation tests, CTM, HIV, Glucose, ALT, AST, Bilirubin, Amylase, Creatinine, electrolytes.
Visit with an anesthesiologist to evaluate all factors involved in anesthesia. Explanation: Before performing the procedure, the doctor who orders ERCP/the doctor performing the procedure must fully explain to the patient and the patient's family about the procedure, the benefits of the procedure, and the risks. Possible complications, alternatives (if any), limitations of the procedure and methods of preparation. A written consent to endoscopy should be signed by the patient or the patient's family after being explained.

Thực hiện xét nghiệm đông máu cơ bản trước khi tiến hành thủ thuật
5. Is ERCP safe? Complications and how to detect complications?
ERCP is a relatively safe and minimally invasive procedure, but it can also have the following complications:
Duodenal, biliary tract bleeding: May occur, especially when removing the sphincter of Oddi. Bleeding is usually minor and will go away on its own. If this occurs during the procedure, it can be treated with endoscopic techniques, such as hemostatic clamps, injection of epinephrine (a vasoconstrictor), or the use of an electrocautery. Very rarely, severe bleeding requires surgical intervention. If bleeding after intervention, common signs are fatigue, dizziness, dizziness, pale skin, pale mucous membranes, rapid pulse, low blood pressure, vomiting blood or black stools. Acute pancreatitis occurs within 24 to 48 hours of ERCP. The telltale signs are abdominal distension, severe abdominal pain in the left epigastrium. Most cases of pancreatitis after ERCP are mild, but rarely it can become serious and life-threatening. Duodenal or biliary tract perforation: This is a rare complication, if the perforation is small, there is no peritonitis, it can be treated endoscopically such as suturing the hole with Clip clips, medical treatment: fasting, antibiotics. birth, closely monitored, a few can become serious and even require surgery. Early signs are severe abdominal pain immediately after the intervention, can palpable air under the skin, there may be difficulty breathing if there is a lot of pneumothorax or pneumomediastinum. Biliary tract infections (cholangitis, cholecystitis) can occur, especially when the bile ducts are not drained well, the obstruction has not improved, or in a patient with an existing infection. Common symptoms of high fever, chills, abdominal pain, fatigue, chills, loss of appetite, dark urine, etc. Aspiration can occur when food from the stomach backs up and is inhaled into the airways, causing difficulty breathing. or pneumonia. Patients who have fasted for several hours prior to the procedure minimize this risk. The overall rate of complications is from 5-7% of ERCP cases, the mortality rate is only 0.3%.
Sau ERCP bệnh nhân có thể gặp phải biến chứng viêm tụy cấp
6. Length of hospital stay, notes on when you go home from the hospital?
After ERCP intervention, the patient must stay in the hospital for monitoring and treatment, usually 2 to 3 days, if there are no complications, they can be discharged.
When you go home, if you see the following signs, you should contact your doctor immediately:
Fever or chills, shortness of breath, chest pain; Abdominal pain, severe abdominal distension, hard and painful to touch; Vomiting; Difficulty swallowing; A 'cracking' feeling under the skin; Bleeding (stools containing fresh, dark brown or black blood, or vomiting blood). If there is no abnormal development, the patient should re-examine under the guidance of the doctor to discuss and monitor the disease.
To ensure safety, you should perform this technique at reputable and quality hospitals.
References:
ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, et al. Adverse events associated with ERCP. Gastrointest Endosc 2017; 85:32. Andrea Tringali, MD, PhD; Silvano Loperfido, MD; Guido Costamagna, MD, et al. Endoscopic retrograde cholangiopancreatography: Indications, patient preparation, and complications. Update - Last updated: Apr 02, 2020.