This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Nguyen Quoc Viet - Interventional Cardiologist - Department of Examination & Internal Medicine - Vinmec Danang International HospitalCoronary heart disease ECG will provide indirect information about the presence, extent and extent of some coronary diseases. Recent studies that have analyzed ST segment changes provide useful information in acute coronary syndromes with myocardial infarction.
1. Electrocardiogram in myocardial ischemia
Myocardial ischemia will lead to a decrease in the resting membrane potential (from -60 to -65 mV), resulting in a decrease in the rate of rise of phase 0, a decrease in the amplitude and duration of the potential work.
The effect of myocardial ischemia on the electrocardiogram is the damage current. This injury current is generated from local depolarization combined with a shortening of the action potential, resulting in a potential difference between the anemic cells and the adjacent normal cells. These physiological abnormalities will produce damage currents during both systole and diastole and ST-segment elevation patterns on the electrocardiogram.
When there is transmural ischemia, early repolarization occurs (phase 2 and phase 3), leading to anemia cells will be more negative than normal cells. The current in the cell will go from the normal cells to the anemic cells (in the direction from positive to negative). From there, the ST segment vector will be directed towards the epicardial layer, resulting in ST segment elevation and T wave elevation in ischemic sites on the ECG.
In cases where the ischemia is limited to the subendocardial layer, the ST segment vectors will be directed towards the endocardial layer, causing ST segment depression in the ischemic regions on the electrocardiogram.
2. Electrocardiogram of acute myocardial infarction
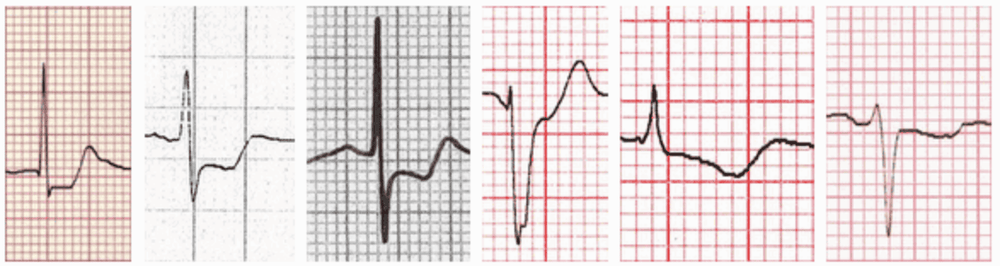
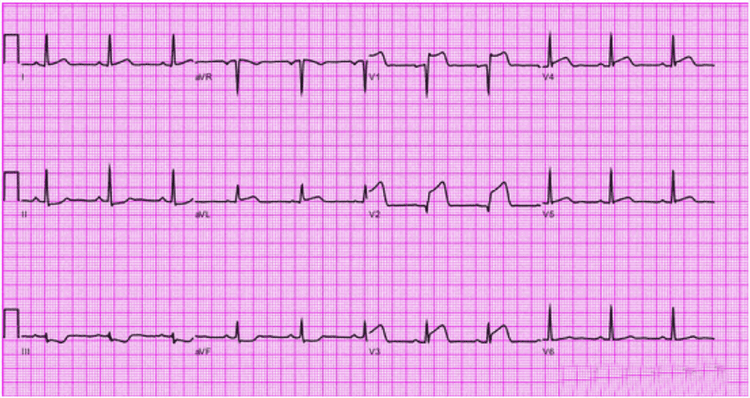
2.1. ST-elevation myocardial infarction When a coronary artery is blocked, the heart muscle is more severely ischemic leading to damage and eventually necrosis. On electrocardiogram, the manifestation of ischemia is the change of the T wave, the manifestation of injury is the ST segment elevation, the manifestation of necrosis is the appearance of the Q wave. The Q wave is only significant. pathology when ≥ 0.04 s wide or higher than 1⁄4 R waves, respectively. Kinetic changes of ST segment, T wave and pathological Q wave in acute myocardial infarction :
fulminant phase: High, sharp T waves appear minutes to hours after the onset of angina pectoris, signs This is usually transient and goes away very easily. Acute phase: ST segment elevation with elevation in amplitude of the QRS complex and vertical T waves. ST-segment elevation usually resolves within a few hours to a few days, and rarely over several weeks. If after 2 weeks ST segment elevation is still present, ventricular aneurysm problems or abnormal ventricular motor function should be considered. Pathological Q waves can appear about 2 hours after an angina attack and develop fully within 9 hours. In most patients, pathological Q waves will persist indefinitely, but in about 6-20% of patients, Q waves may return to normal within 1-2 years. Within 12 hours of onset, the ST segment elevation should subside rapidly, at which point the T wave begins to reverse early, even earlier than ST segment normalization. T waves will disappear within days to weeks or may persist indefinitely. Normalization of negative T waves often reflects motor restoration of the heart wall.
2.2 . Non-ST-elevated myocardial infarction The electrocardiogram findings of a non-ST-elevated myocardial infarction range from a normal ECG or non-specific ST-T changes, to ST segment depression and T wave inversion.
3. Electrocardiogram criteria in the diagnosis of acute myocardial infarction
ST elevation: New J-point elevation (J-score is used to determine the degree of ST-segment elevation) in two contiguous leads with a cutoff ≥0.1mV (1mm) in all leads. Particularly in V2-V3, the cut-off point was ≥0.2 mV in men ≥40 years old, ≥0.25 mV in men <40 years old, or ≥0.15 mV in women. ST depression and T-wave change: new horizontal ST depression or down-sloping ST 0.05 mV in two adjacent leads, and/or T-wave inversion ≥0.1 mV in two adjacent leads with R waves occupying dominant or R/S ratio >1. Occasionally, myocardial ischemia can produce a qualified ST-segment change in one lead, but may be slightly less in the adjacent lead. Lesser ST-segment changes or T-wave inversions cannot rule out acute myocardial ischemia or associated myocardial infarction, because recording a single ECG may miss dynamic ECG changes, which can be detected by serial ECG recording.Electrocardiographic evidence of myocardial ischemia in the region of the circumferential coronary artery is often overlooked; transitions V7, V8, and V9 should be recorded when clinically suggestive of CRC (electrocardiogram). Initial imaging is undiagnosed or ST depression in V1-V3).
The ST-segment elevation cutoff point in V7-V9 is 0.05mV, for men <40 years the cutoff point is raised to ≥0.1 mV.
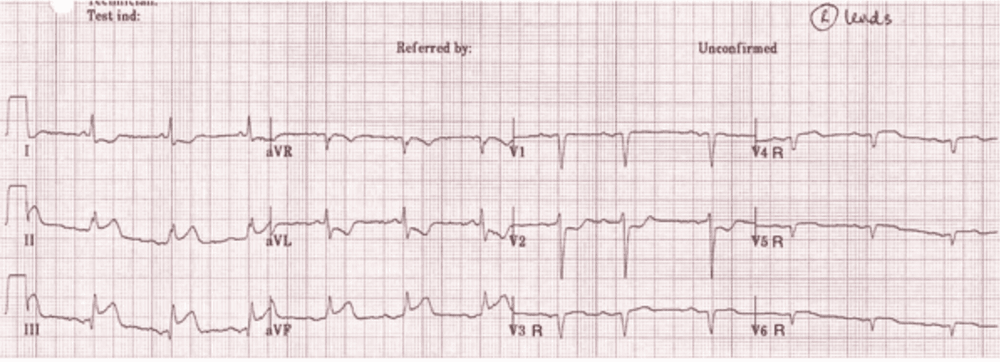
In patients with inferior MI with signs suggestive of RV MI, leads V3R and V4R should be recorded, because ST elevation ≥ 0.05 mV (≥ 0.1 mV in men < . 30 years) were the supporting criteria for the diagnosis.
Transient Q waves may be present during the acute phase of myocardial ischemia or greater in acute myocardial infarction with successful reperfusion.
Diagnosis of myocardial infarction is more difficult in the presence of left bundle branch block. However, consistent ST-segment elevation or a pre-existing ECG is helpful in determining the presence of myocardial infarction. In patients with right bundle branch block, ST-T abnormalities in leads V1-V3 are common, making it difficult to identify ischemia in these leads, but when ST is present. elevation or Q wave, the diagnosis of myocardial infarction should be mentioned.
Today, the relationship between the electrocardiogram image and the location of coronary artery damage in acute myocardial infarction has been determined by many studies. Coronary ECG can help predict coronary artery damage, help early reperfusion, and prepare resuscitation facilities for patients with acute myocardial infarction.
Currently, Vinmec International General Hospital has applied electrocardiogram technique in examination and diagnosis of many cardiovascular diseases and diseases related to coronary arteries. Electrocardiogram testing at Vinmec International General Hospital is carried out methodically and in accordance with standard procedures by a team of highly qualified medical professionals, modern machinery and standard equipment, thereby giving electrical results. Accurate ECG contributes significantly to the identification of the disease and the stage of the disease in order to have the most effective treatment regimen.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.