This is an automatically translated article.
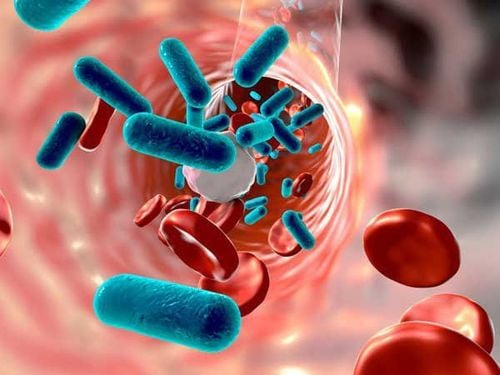
The article was written by Master - Doctor Mai Vien Phuong - Head of Department of Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalSepsis is a potentially life-threatening condition that occurs when the body's response to an infection damages its own tissues. When infection-fighting processes take place in the body, they cause the organs to function poorly and abnormally. Sepsis can progress to septic shock.
1. Overview
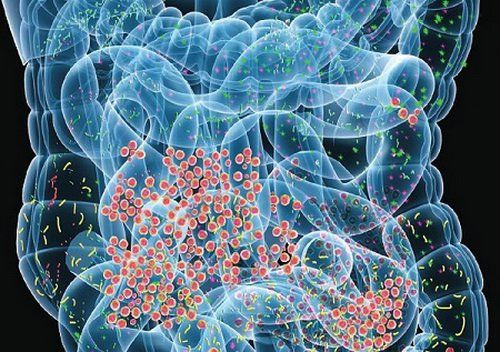
Sepsis refers to life-threatening organ dysfunction caused by an imbalanced response to an infection. As the largest reservoir of bacteria and endotoxins in the body, the intestinal tract is considered the "engine" of sepsis and multi-organ dysfunction syndrome. Under normal circumstances, the gut microbiota plays beneficial roles in the human immunological and physiological context, existing in a homeostasis important for the maintenance of human health. .
However, in severe disease, homeostasis is disrupted, leading to abnormal changes in the type, number, proportion and location of microorganisms in the intestinal tract, thereby increasing susceptibility to sepsis. In fact, studies have shown that there is a dose-response relationship between the degree of intestinal dysbiosis and the incidence of subsequent severe sepsis. Therefore, it is of great significance to improve understanding of the status and extent of intestinal microbiota disturbances in patients with sepsis. For example, the establishment of powerful gut microbiota-based biomarkers will enable accurate prediction of the prognosis of sepsis patients and, as a result, the application of appropriate therapeutic measures. However, there are few reports on the gut microbiota associated with sepsis and its dynamic changes. High-throughput 16S rRNA gene sequencing enables a comprehensive understanding of the gut flora structure and is the standard technology used to analyze the human gut microbiota. In many studies, the diversity and composition of the gut microbiota in patients with sepsis, patients without sepsis and healthy subjects were analyzed and compared. Dynamic changes in the diversity and structure of the gut microbiota over the course of 1 week [1, 3 and 7 days after admission to the intensive care unit (ICU)] were also studied to reveal Variation of gut microbiota in the context of antibiotic therapy. In addition, potential relationships between gut microbiota imbalance and clinical indicators in sepsis were investigated through correlation analysis.
2. What do the studies show?
The authors enrolled 10 patients with sepsis (sepsis group) hospitalized at the Health Care Department of General Hospital, Ningxia Medical University, China (class IIIa general hospital). from February 2017 to June 2017; 10 patients without sepsis hospitalized during the same period (non-sepsis group) and ten healthy people (control group) were also enrolled.Stool samples collected from three groups were sequenced with 16S rRNA genes and determined the diversity, structure and composition of gut flora. In addition, the dynamics of the diversity, structure, and composition of the gut microbiota in sepsis patients were investigated through 16s rRNA gene sequencing of samples collected 0 days, 3 days and 7 days after admission to the intensive care unit. The correlation between the serum levels of procalcitonin, endotoxin, diamine oxidase, and D-lactic acid and the composition of the gut microbiota of patients with sepsis was also investigated. Compared with healthy controls, sepsis and non-sepsis patients showed reduced gut microbiota diversity and distinct flora structure, with Firmicutes being the dominant species and prevalence of bacteria. significantly reduced strains in Bacteroidetes, as well as Prevotella and Lachnospira, among other genera.
Notably, the incidence of Enterococcus was significantly increased in the intestinal tract of patients with sepsis. Interestingly, the diversity in the sepsis group decreased gradually, from day 1 to day 7 of treatment. However, pairwise comparisons showed that neither the diversity and structure of the gut microbiota were significantly different when considering the three different time points studied. Curiously, serum levels of procalcitonin, endotoxin, diamine oxidase and D-lactic acid in patients with sepsis correlated with the prevalence of different bacterial genera. For example, Ruminococcus prevalence is positively correlated with serum procalcitonin, endotoxin, and diamine oxidase. Similarly, the rate of Roseburia was positively correlated with serum procalcitonin, endotoxin, and D-lactic acid.

3. Structural characteristics of intestinal microbiota in patients with sepsis
Sepsis is associated with high morbidity and mortality worldwide, making timely identification and treatment difficult. Therefore, improving the diagnosis and treatment of sepsis is essential from a global health point of view. In February 2016, SCCM and the European Society of Intensive Care Medicine jointly defined sepsis as follows: “Sepsis is a life-threatening organ dysfunction caused by the response of The host is dysregulated to infection”. This definition emphasizes the close relationship between sepsis and organ dysfunction. It should be noted that the intestinal tract is considered as the "engine" causing dysfunction of the organs. The gut microbiota, which is an important component of the gut, plays a key physiological role in the context of biosynthesis and metabolism. However, serious diseases lead to many changes in the diversity of the gut microbiota, causing an overgrowth of pathogenic bacteria. There are marked differences in the abundance, distribution and structure of the gut microbiota in the setting of sepsis: By comparing the gut microbiota of sepsis patients and healthy controls, The authors confirmed that there are marked differences in the abundance, distribution and structure of the gut microbiota in the setting of sepsis. In patients with sepsis, normal bacteria decrease or disappear, while the abundance of abnormal bacteria increases sharply.At the phylum level, Firmicutes abundance was significantly increased, while Bacteroidetes bacteria were significantly decreased in the gut microbiota of sepsis patients compared with non-infectious critically ill patients. Of note, the number of bacteria in the phylum Fusobacterium was also significantly reduced.
At the genus level, in addition to a decline in the number of beneficial symbiotic bacteria such as Prevotella and Lachnospira, as well as other genera, including Fusobacterium and Peptostreptococcus. The authors found that Enterococcus abundance was significantly increased in the gut microbiota of patients with sepsis compared with critically ill patients without infection. Thus, the authors' results suggest that sepsis dysbiosis exhibits three main features.
First, as the abundance and diversity of the gut microbiota decreases, the structure of the gut microbiota changes and the inter-individual variation is greater. Second, the abundance of dominant obligate anaerobes decreased and the number of preferred anaerobes increased. Third, a decrease in the abundance of beneficial bacteria, while an increase in pathogenic bacteria, may become dominant. The occurrence of intestinal microbiota disturbances in patients with sepsis: The occurrence of intestinal microbiota disturbances in patients with sepsis is not surprising. First, the physiological state of sepsis patients is completely different from that at homeostasis. In particular, intestinal hypoperfusion and reperfusion injury leads to changes in the intestinal environment and blood supply to the intestinal mucosa, leading to inflammation of the intestinal mucosa and consequent series of changes in the intestinal environment. Such as increased nitrate concentration and altered mucosal oxygen gradient.
These changes favor the growth of Proteobacteria, leading to the growth of many clinically familiar Gram-negative bacilli, such as Pseudomonas aeruginosa and Escherichia coli, as well as Staphylococcus aureus and Enterococcus. Second, ICU patients are exposed to various endogenous regulators (such as increased catecholamine production and altered glucose metabolism) and clinical interventions (such as proton pump inhibitors, opioids, supportive care). nutrients and antibiotics), affects the habitat of the gut microbiota to varying degrees and, thus, affects the flora structure. Eventually, the intestinal mucosa will be damaged and thinned in critically ill patients; Such mucosal damage leads to loss of the normal habitat of symbionts, which, in turn, leads to intestinal dysbiosis.
The authors' study showed that the abundance, distribution, and diversity The profile of the gut microbiota in patients with sepsis did not change significantly within 1 week of ICU admission. However, regarding the gut microbiota of healthy individuals, the numbers of most beneficial bacteria, such as Prevotella and Bifidobacterium, were below the limit of detection in patients with sepsis. While the abundance of bacteria associated with infection, such as Enterococcus and Haemophilus, increased despite the effects of antibiotics (with the exception of Coprococcus, which decreased abundance below the detection limit).
These results indicate that patients with sepsis-associated gut microbiota are unlikely to recover in a short time and while the drug is effective against the bacteria causing the infection, They also affect the bacteria in the gut. In fact, the effects of drug treatment, especially antibiotics, on bacteria are not limited to harmful bacteria; The percentage of beneficial bacteria in the gut also decreased.
Long-term antibiotic use alters the normal healthy gut microbiota and leads to the emergence of resistance:
Other studies have also shown that long-term antibiotic use long-term changes in the normal healthy gut microbiota and leads to the emergence of drug resistance. Worryingly, the long-term use of antibiotics has the potential to create reservoirs of organisms with multidrug-resistant genes. Ma et al used a mouse model of third degree burns over 30% of the total surface area of the back and quantified/identified gut bacteria after treatment. The results showed that the number of cocci in the gastrointestinal tract of rats was significantly increased, and the cocci/bacilli ratio was severely reversed after treatment with Rocephin. It is thought that broad-spectrum antibiotics have disrupted the balance of intestinal microflora. Note that the pathogenic gut microbiota has the potential to affect health, disease and drug effects. The authors' study also revealed that Enterococcus abundance was significantly increased in sepsis patients, which may be related to the use of broad-spectrum antibiotics.
Above is some information about the effect of sepsis on the structure of the gut microbiota. Please follow the website: Vinmec.com regularly to update many other useful information.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Yang XJ, Liu D, Ren HY, Zhang XY, Zhang J, Yang XJ. Effects of sepsis and its treatment measures on intestinal flora structure in critical care patients. World J Gastroenterol 2021; 27(19): 2376-2393 [DOI: 10.3748/wjg.v27.i19.2376]