This is an automatically translated article.
Article by Doctor Le Van Binh - Department of Critical Care - Vinmec Times City International Hospital.Newborns with severe respiratory failure, if not detected and treated promptly, will lead to extremely serious complications, even life-threatening. This is a very common disease, so parents need to monitor the baby's breathing for at least 7 days after birth to promptly detect any abnormality.
1. Definition of respiratory failure
To put it simply, respiratory failure is an inability to adapt the respiratory apparatus of the human body. Respiratory distress in infants may appear soon after birth or several hours/day later. This is a very common disease, so parents need to monitor the baby's breathing for at least 7 days after birth to promptly detect any abnormality.Normally newborns breathe 40-60 times/minute. Newborns, especially premature babies, have short breaths of less than 15 seconds. However, if the apnea lasts > 15 seconds, repeated many times, it will easily lead to respiratory failure.
Symptoms to evaluate the child's respiratory function according to the Silverman index include:
|
Điểm Chỉ số |
0 | 1 |
| Di động ngực - bụng | Cùng chiều | Ngực < bụng |
| Co kéo cơ liên sườn | 0 | + |
| Rút lõm hõm ức | 0 | + |
| Cánh mũi phập phồng | 0 | + |
| Thở rên | 0 | qua ống nghe |
Below 3 points: The child does not have respiratory failure; From 3-5 points: Mild respiratory failure; Over 5 points: Severe respiratory failure.
2. Symptoms of respiratory failure in infants
2.1. Clinical Newborns with respiratory failure will show some main signs such as:Fast breathing rate over 60 times/minute or slow breathing rate less than 40 times/minute; Contraction of the intercostal muscles, above and below the sternum, thoracic abdominal breathing moves in the opposite direction; Purple around lips, extremities, whole body. Cyanosis occurs when the PaO2 in the blood falls below 70 mmHg or the reduced hemoglobin is above 5g%. Signs suggestive of respiratory failure in children:
Unbalanced chest; Vocal vibration increases in pneumothorax; Percussion in pleural effusion; Pay attention to find the beating position of the apex, if there is a change in position, think of either pneumothorax, or diaphragmatic hernia; Heart murmur, palpation of the inguinal artery (mainly in case of ductus arteriosus), hepatomegaly in heart failure... Effects of severe respiratory failure on other organs:
Arrhythmia (rapid) more than 160 times/minute or less than 100 times/minute). Cardiac arrest if blood PaO2 drops significantly, below 30 mmHg; Brain: Hypoxia is manifested by clinical symptoms such as restlessness, lethargy, decreased or lost muscle tone, convulsions; Urology: Oliguria or anuria due to acute renal failure. 2.2 Measurement of blood gases To determine the severity of respiratory failure and acid-base disorder in children, the following method can be used:
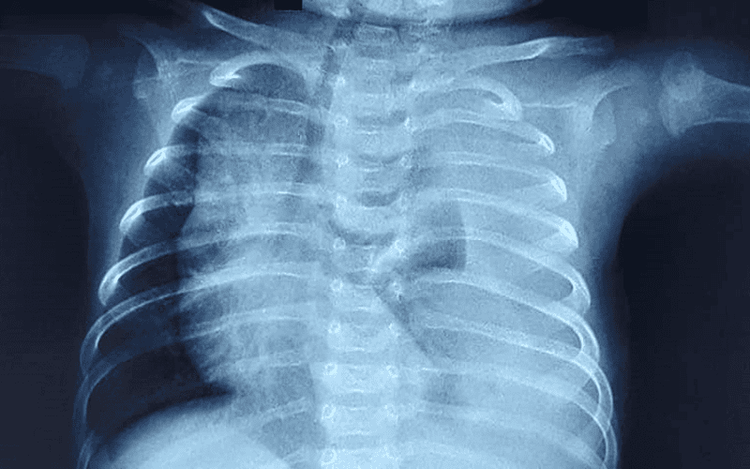
Measurement of oxygen concentration through the skin, this method is easy to perform and can adjust the oxygen concentration of inhaled air to suit the child. Measure gases, pH of arterial blood to see the degree of respiratory failure: If Pa02 falls below 50 mmHg, PaC02 rises above 70 mmHg, pH falls below 7 will appear complications such as intermittent apnea, cerebral edema , cerebral hemorrhage... 2.3. Chest radiograph is an important and indispensable technique in the diagnosis of respiratory failure in neonates. It is best to shoot at bed. Usually straight chest x-ray, in case of suspected pneumothorax, put the child on the healthy side and give the beam parallel to the horizontal plane to make the diagnosis easier.
3. Causes of severe respiratory failure in infants
3.1. Due to upper airway obstruction Posterior nostril obstruction; Esophageal-tracheal intubation; Pierre - Robin syndrome : The tongue does not have a brake, so it is easy to fall back in the supine position and cause upper airway obstruction; Throat polyps; Laryngeal stenosis due to edema, soft cartilage of the larynx. 3.2. Causes in the lungs Lung malformations such as: Congenital cocoon, lung atrophy, pneumothorax; Young lungs; Aspiration syndrome of amniotic fluid meconium ; Endothelial disease ; Pulmonary fluid retardation syndrome; Lung infection; Lung collapse; Pneumothorax, mediastinum; Pulmonary hemorrhage. 3.3. Congenital heart Transversion of the great arteries; Left ventricular dysfunction; Aortic stenosis; Fallot 4, especially with left ventricular failure. 3.4. Abnormalities of the thoracic cavity Porak Durant. 3.5. Abnormalities of the respiratory muscles Diaphragmatic hernia; Werdnig-Hoffman syndrome: The disease is familial and inherited. It is a state of motor cell dysfunction of the brain causing total muscle tone reduction, fetal movement little, crying inaudibly, poor feeding, and lack of movement after birth; Myasthenia gravis primary or secondary due to neuromuscular damage, decreased acetylcholine secretion: Babies born cry weak, difficult to suckle, easy to choke, prone to severe respiratory failure ... 3.6. Blood diseases Hemolytic anemia (mother-child blood group incompatibility), hemorrhage; Polycythemia vera; Blood clotting disorder. 3.7. Due to the brain Cerebral edema ; Brain hemorrhage; Brain damaged; Encephalitis - meningoencephalitis; Sedatives, anesthetics used for mothers before giving birth. 3.8. Metabolic disorders Acidemia; Hypoglycemia; Hypocalcemia.
4. Principles of treatment of severe respiratory failure in children
4.1 Oxygen therapy Indications: When Pa02 falls below 70 mmHg in arterial blood or when the child is cyanotic.Principle:
Oxygen therapy must be performed rapidly to raise Pa02 to 100mmHg. Before breathing oxygen, pay attention to sucking sputum from the nose and throat to ensure a clear airway for the child. Ensure the humidity of inhaled oxygen is 80-90% with steam or pass through clean water, the appropriate oxygen concentration is from 30-40% to 100% if cyanosis is much. When the baby's cyanosis is gone, gradually reduce the oxygen concentration to normal (21%). Pay attention to warming the inhaled air to body temperature. Method of providing oxygen to the child:
The nasal tube is used when the child can breathe on his own, has 30-40% oxygen demand, the flow is 1l/min. Mask applied to the nose - mouth used when the child has a need for oxygen and needs respiratory aid. Through the mask, the child can breathe 30-40% oxygen with a flow of 5 l/min or 100% with a flow of 10 l/min. Squeeze the ball at a frequency of 40 times/minute. Select a mask that fits the patient's face size. Tent: Used when the patient is breathing on their own, the oxygen concentration is 30-40% with a flow of 5l/min or 100% with a flow of 10l/min. Ventilators are indicated when the patient stops breathing for a long time and recurs, balloon compression is not effective. The patient was intubated and mechanically ventilated with a positive pressure of 20-30 cmH20. Caring for the patient on oxygen:
The patient must be placed with a pillow under the back to straighten the airway; Suction sputum regularly, the straw must be sterile; Change the patient's position, vibrate the lungs to avoid sputum sputum, atelectasis; Ensure body temperature 36.5-37 °C; Sedatives can be used if the child is irritable or agitated. Monitoring oxygen patients:
To assess the effectiveness of oxygen therapy, it is necessary to monitor breathing rate, pulse, temperature, heart rate, skin color, chest movement, measure Pa02, PaC02, blood pH . Ensure oxygen saturation between 85-95% to avoid complications of oxygen toxicity. If after 30 minutes of oxygen breathing, the child's cyanosis ceases to be, and the pink color returns, indicating that Pa02 has returned to normal, we gradually reduce the oxygen concentration in the inhaled air. If, after that time, the patient is still cyanotic, the pulse is still rapid and small, indicating that oxygen therapy has not been effective, it is necessary to find and address the interfering causes, usually heart failure, acidosis, or lung injury. If the patient breathes oxygen for more than 24 hours, it is necessary to monitor the oxygen concentration in the inhaled air and in the arterial blood because it can cause oxygen toxicity if Pa02>150mmHg persists for more than 24 hours (atrophy of the retina). in premature infants, bronchopulmonary dysplasia causes chronic respiratory failure in children using ventilators for a long time). 4.2 Treatment of acidosis When there is a metabolic acidosis, use sodium bicarbonate 14‰, 42‰ solution. The amount of infusion was calculated by the formula: Number of mEq = BE x P (kg) x 0.3.
In case of respiratory acidosis (PaC02 >70mmHg), use a ventilator to treat.
In the case of "finding" we use Sodium Bicarbonate 14 ‰, 10-15 ml/kg (1 mEq/kg).
4.3. Treatment of exhaustion Provide adequate energy to the child orally or intravenously.
4.4. Treatment of infections Treat infections in children with severe respiratory failure with broad-spectrum antibiotics.
5. ECMO in infants

Indication of ECMO in neonates in the following cases
Diaphragmatic hernia; Meconium aspiration syndrome; Persistent pulmonary hypertension (PPHN); Pneumonia/ Sepsis; Endothelial disease; ARDS . Criteria: Based on predictive indicators of mortality over 80%:
Children > 34 weeks of gestation; Weight >2kg; No coagulopathy or uncontrolled bleeding; No cerebral hemorrhage grade II or higher; Do not ventilate 100% oxygen for more than 14 days; Reversible lung disease; There are severe deformities; There is no heart disease that cannot be treated; Prolonged Hypoxia: Oxygen Index (OI >=40 lasting 2-4 hours). ECMO is contraindicated in neonates in the following cases:
Diseases beyond the lungs, the heart cannot be treated; Severe, irreversible multiple organ failure; Grade 2-4 intracranial bleeding; Coagulopathy or uncontrolled bleeding. As soon as the child shows symptoms of severe respiratory failure, parents need to take the child to a reputable hospital to be consulted by a specialist for monitoring and treatment. Currently, the Pediatrics Department at Vinmec International General Hospital is trusted by many parents to examine the diseases that infants and young children are susceptible to. Vinmec brings satisfaction to customers and is highly appreciated by industry experts by:
Gathering a team of leading pediatricians: Including leading experts with high professional qualifications ( professor, associate professor, doctorate, master), experienced, worked at major hospitals such as Bach Mai, 108.. The doctors are well-trained, professional, have a heart - a vision. Understanding young psychology. In addition to domestic pediatric specialists, the Department of Pediatrics also has the participation of foreign experts (Japan, Singapore, Australia, USA) who are always pioneers in applying the latest and most effective treatment regimens. . Comprehensive services: In the field of Pediatrics, Vinmec provides a series of continuous medical examination and treatment services from Newborn to Pediatric and Vaccine,... according to international standards to help parents take care of their baby's health from birth to childhood. upon reaching adulthood. Advanced techniques: Vinmec has successfully deployed many specialized techniques to make the treatment of difficult diseases in Pediatrics more effective: neurosurgery - skull surgery, hematopoietic stem cell transplantation in cancer treatment. Professional care: In addition to understanding children's psychology, Vinmec also pays special attention to the children's play space, helping them to play comfortably and get used to the hospital's environment, cooperate in treatment, improve the efficiency of medical treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.