This is an automatically translated article.
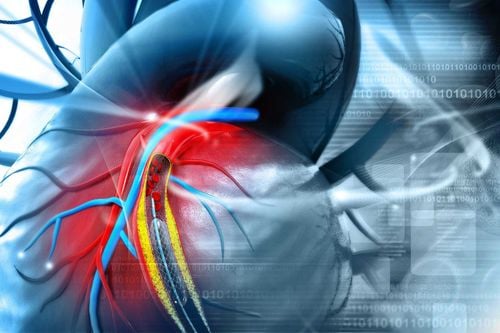
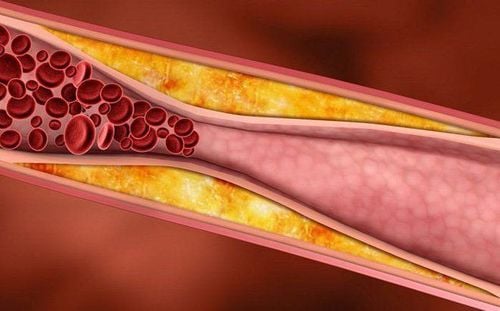
Current treatment methods for coronary artery disease include medical treatment, intervention and surgery. Percutaneous coronary intervention is a non-surgical treatment that both relieves symptoms and resolves the cause of the narrowing of the artery.Video content is consulted by Master, Doctor Do Xuan Chien - Department of Medical Examination and Internal Medicine - Vinmec Ha Long International Hospital
Percutaneous coronary intervention is indicated in the treatment of coronary artery disease, specifically:
Stable angina unresponsive to medical treatment; Stable angina, myocardial ischemia (positive stress test or positive myocardial perfusion scan) and coronary artery disease supplying a large area of myocardium; Unstable chest pain/acute myocardial infarction without ST-segment elevation but high risk stratification; In case of acute myocardial infarction with ST elevation; Angina appeared after the patient performed coronary bypass surgery. After percutaneous coronary intervention, there were symptoms of restenosis. Percutaneous coronary intervention is done by simply opening a small hole in the skin to insert a small catheter (catheter) into an artery in the thigh or wrist. Patients only need local anesthesia, not anesthesia like open surgery, so the patient remains awake and does not feel pain during the procedure. The stenting process is quick, within about an hour, and most patients can go home in 1-2 days. Angioplasty and percutaneous coronary stenting help to resolve the narrowing and blockage in the coronary arteries, improve blood flow to the myocardium, and allow the patient to function normally without angina.
Percutaneous coronary intervention is an invasive procedure, so there may be complications such as:
Infection (low rate); Perforation, laceration of coronary artery causing pericardial effusion; Cardiac arrhythmias; Heart stop; Stent occlusion causes myocardial infarction after stenting. Complications after coronary intervention have a very low rate. There are also cases of patients who are allergic to contrast after the intervention. Before the intervention, the doctor will take the patient's history, if there is a history of drug or seafood allergy, allergy prophylaxis will be given before the intervention. After the intervention, to prevent kidney failure due to contrast, the doctor will give enough fluid for the patient.
After the procedure, the patient should rest at bed, if radial intervention (wrist puncture), the hand should be raised and the hand should be stabilized to help stop bleeding better. If the femoral artery is inserted, the patient should be immobilized for 6 to 8 hours, especially the leg on the side of the procedure to ensure that the puncture has stopped bleeding. Remember to hold the puncture site when you cough or sneeze. Call your nurse immediately when you notice recurrent bleeding or pain in multiple areas of the artery. Patients should drink more water to prevent hypotension and kidney disease due to the effect of contrast agents.
In summary, percutaneous coronary intervention is a difficult technique, requiring medical facilities to have a team of highly qualified and experienced doctors and nurses in the field of Cardiology and medical facilities. quality, modern equipment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.