This is an automatically translated article.
The article was written by MSc Le Thi Na - Doctor of Hematology, Laboratory Department - Vinmec Times City International General Hospital.
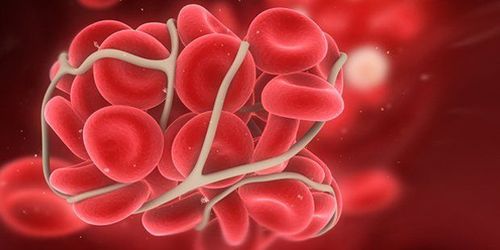
Disseminated intravascular coagulation syndrome occurs due to excessive thrombus formation in the lumen, accompanied by the conversion of fibrinogen to fibrin in the microcirculation. Disseminated intravascular coagulation syndrome can cause dangerous complications if not treated properly.
1. Definition
Disseminated intravascular coagulation (DIC), also known as coagulopathie de consummation, is a medical condition caused by the formation of too many blood clots (thrombose) in the blood vessels. vessels, accompanied by the conversion of fibrinogen to fibrin in the microcirculation. Biologically, this is consumptive coagulation, meaning that coagulation factors are absorbed and used up in the formation of thrombin and fibrin. Clinically, this is a phenomenon of bleeding due to a lot of clotting, which means that there are two manifestations at the same time: coagulation syndrome and bleeding syndrome.2. Pathogenesis
The cause of the onset of disseminated intravascular coagulation syndrome is an excessive increase in thromboplastin activity in the blood, which activates coagulation, forms thrombin, and converts fibrinogen into fibrin in the microvasculature. As a result, there is an overconsumption of fibrinogen, prothrombin, factors V, VIII and platelets, and the activation of factors VII, IX, X, and XII, which is more likely to occur secondary to fibrinolysis due to The fibrinolytic system is activated and the production of fibrinogen and fibrin degradation products is increased. Coagulation disorders occur due to:
There is penetration into the blood of substances with thromboplastin activity of destroyed tissues (broken tissues, broken red blood cells, destroyed cancer cells, amniotic fluid). , lipids derived from hemolysis, bacterial endotoxins, ...) There is a role of bradykinin, kallikrein, histamine, of the antigen-antibody complex, of platelet agglutinating factors such as thrombin , proteolytic enzymes, ADP, catecholamines, serotonin, collagen, prostaglandins, thromboxane, thrombomodulin, tissue plasminogen activating factor (tPA), plasminogen activator inhibitor I (PAI-I). There is also a role for tumor necrosis factor (TNF), interleukins 1 and 8, leucotriene B4 and platelet activating factor (PAF). There are factors that favor the decline of the inhibitory systems of coagulation such as reduction of antithrombin plasma as in cirrhosis, in the blockade of the retinal system due to pregnancy, long-term treatment with high-dose corticosteroids. There are aggravating factors: circulatory failure, acidosis, hypoxia, slow microcirculation, decreased protein synthesis in shock causing decreased production of hemostatic factors that have been consumed by disseminated coagulation syndrome intravascular waste.
3. Diagnosis
Acute form (manifested by massive bleeding, shock): Based on tests
PT (prothrombin time) prolonged. TT (thrombin time) is prolonged. Prolonged activated partial thromboplastin time (APTT). Fibrinogen decreased. Decreased platelets. Red blood cells are broken into pieces. FDP (fibrinogen degradation product) increased. D dimer increased. Diagnosis according to ISTH 2009 (clinical and kinetics)
| Điểm | 0 | 1 | 2 |
| Số lượng tiểu cầu | >100 G/L | < 100g/L | < 50G/L |
| PT kéo dài | < 3 giây hoặc > 70% | 3 giây < PT< 6 giây hoặc 40% ≤ PT ≤ 70% | < 6 giây hoặc < 40% |
| Fibrinogen | >1g/L | < 1g/L | |
| D dimer so với giới hạn cao bình thường | < 2 lần | 2-5 lần | >5 lần |
>5 points: clear DIC, daily lab check to monitor progress; < 5 points: DIC is not clear, need to follow up 1-2 more days if clinical manifestations are suspicious of DIC. It should be noted that the presence of the thrombin-AT III complex and of the plasmin-anti-plasmin complex means that both the coagulation and fibrinolytic systems are active.
Chronic form: In this case, the tests are positive erratically
The platelet count is only slightly decreased, red blood cell fragments (+). Fibrinogen is elevated or normal. PT and APTT are normal, FDP and D dimer are usually high. Disseminated intravascular coagulation and primary fibrinolysis: Both the coagulation and fibrinolysis systems are activated independently of each other, which means that thrombin and plasmin are formed simultaneously. Common laboratory abnormalities are:
Hemolysis. Time to digest euglobulin Von Kaulla (+). FDP/D dimer is high. In fact, distinguishing between primary and secondary cases is difficult to diagnose. Despite these difficulties, in clinical practice, disseminated intravascular coagulation + fibrinogen and primary fibrinolysis are often seen in the following diseases: pre-myelocytic leukemia, amniotic fluid embolism, prostate cancer with metastasis.
4. Treatment
Treatment of disseminated intravascular coagulation syndrome is very complicated, must combine treatment of systemic causes and symptoms (major bleeding, shock, hemolysis,...) and early treatment. When coagulation has formed: Promptly administer heparin, the first dose is 3000-5000 IU intravenously, then 400-500 IU/kg/24 hours intravenously. Combined with antithrombin III 2 vials/day. The deficiency of coagulation factors should be compensated with fresh blood transfusion, fresh plasma, fibrinogen, platelets.
Using blood products in DIC
Transfusion of platelets when there is clinical bleeding and platelet count < 50G/L or no bleeding but platelet count < 20 G/L; Dosage: Maintain platelet count > 50 G/L.
Infusion of fresh frozen plasma in the presence of bleeding and PT % reduction < 30%; Dosage: 15-20ml/kg/24h, stop infusion when PT ≥ 70%.
Cryoprecipitate factor VIII infusion when fibrinogen < 1G/L dose 2-3 units/24h; Stop infusion when Fibrinogen > 1.5g/L.
Transfusion of red blood cells when Hb < 80 G/L or the patient continues to bleed.
Effective diagnosis and treatment of disseminated intravascular coagulation syndrome allows to reduce mortality, which requires active medical care and adequate supply of laboratory tests and blood products.
Disseminated intravascular coagulation syndrome can cause dangerous complications if not treated properly. Complications can occur in the early stages of the disease, and the absence of clotting factors in the later stages. Complications such as blood clots causing a lack of oxygen to the limbs and organs, stroke, and even excessive bleeding can lead to death.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














