This is an automatically translated article.
Translated and synthesized by Dr. Nguyen Hong Thanh - Vinmec Institute of Stem Cell and Gene Technology
Middle East respiratory syndrome (MERS) for a new strain of corona virus caused in 2012, spread to 27 countries and has up to 34.5% of infections died. There is no specific evidence from clinical trials for any anti-MERS-CoV drugs used in patients with confirmed MERS-CoV infection (WHO 2019 report). Therefore, it is important to protect yourself to prevent infection.
1. How to protect and avoid
Ways to protect and prevent MERS include wearing a mask in public places where there is a high risk of virus infection such as hospitals, piers, bus stations, shopping centers. Carry out hand and foot hygiene, environmental sanitation, disinfection and sterilization of the environment in areas with infected people, avoid direct contact, close contact with infected people for at least 10 days from the date of arrival. the day the symptoms are gone.
Prevention of infection in the community:
Wash regularly with soap or an alcohol-based hand sanitizer with a concentration of 70%. Cover your mouth and nose every time you cough or sneeze, then wash your hands with soap or hand sanitizer as soon as possible. Avoid sharing food, drinks, and eating utensils with an infected person. Regularly clean surfaces with disinfectant solutions. Ensure adequate diet, maintain good ventilation in the home or workplace. Avoid contact and gathering in crowded places, where there is no ventilation.

Thực hiện khử trùng tàu điện ngầm tại Hàn Quốc năm 2015 (nguồn: CNN)
Infection prevention in hospitals:
Organize isolation areas, perform treatment and care for patients with suspected or confirmed MERS-CoV infection. This area must have a red sign saying: "Special isolation area" and detailed instructions hanging at the entrance, with a guard. For at-risk areas where people with MERS-CoV infection are likely to come for initial examination and treatment (respiratory, emergency, medical examination, etc.), a detailed instruction sheet is required. Details are hung at the entrance and have a yellow membrane symbol.
For those suspected of having the disease, do not combine people with confirmed MERS-CoV with suspected people and recommend wearing a mask, washing hands and feet, and limiting contact with others. Sample collection and specialized examination at the bedside should be carried out to avoid spread, and if the patient needs to be moved, appropriate protective equipment should be used.
During the epidemic, limit family members to visit the patient in the hospital, if visiting must wear a mask. Prohibit family members and guests from visiting the isolation ward.
Prevention for medical staff:
Medical staff carrying out patient care and treatment should be equipped with appropriate protective equipment including goggles, face masks, disposable gowns gloves, masks, hats, shoe covers or boots. When performing procedures or providing direct care to patients, medical staff should use N95 masks. Specimens must be placed in a nylon bag or transport box. Wash your hands with soap or an antiseptic solution after coming into contact with respiratory secretions, dirty tools, after caring for the sick, and before leaving the ward or isolation area.
2. Vaccines for MERS-CoV
Some trials are conducted in the laboratory, in animal models or even on a clinical scale with certain drugs and immunosuppressants that are believed to be effective in preventing MERS-CoV .
Some of these drugs include interferon, ribavirin, lopinavir/ritonavir, polyclonal antibodies to MERS-CoV and monoclonal antibodies to protein S, inhibitors of viral RNA synthesis (remdesivir), inhibitors peptide nature (HR2P-M2) and the immunosuppressant mycophenolate mofetil (MMF) (Arabi 2017). However, to date, there is no specific evidence from clinical trials for any anti-MERS-CoV drug to be administered to patients with confirmed MERS-CoV infection (report. WHO report 2019).
A number of vaccine development studies for MERS-CoV have been carried out based on recombinant technology, that is, the expression of the gene region encoding the S protein of the MERS-CoV virus in the Ankara virus origin vector (MVA). . more (Mubarak 2019). In addition, the use of adjuvants together with the above vaccines has the ability to enhance the immunogenicity and protective effect of these vaccines in laboratory mice.
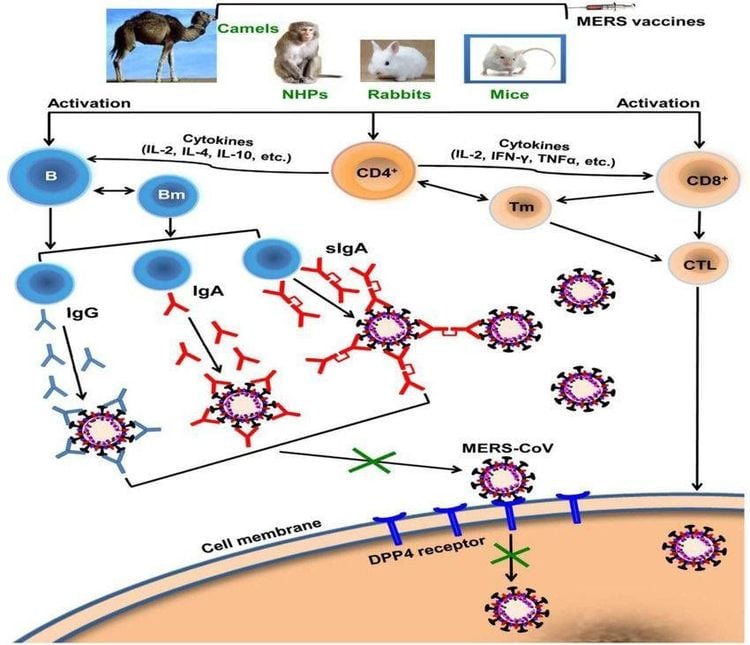
Sơ đồ nghiên cứu chế tạo vắc-xin phòng ngừa MERS-CoV (nguồn: doi: 10.1586/14760584.2016.1167603).
3. Epidemic evolution
September 2012, the first case of MERS-CoV infection was officially confirmed in Saudi Arabia. In November 2012, a study found that the cause of the epidemic in Jordan was also caused by MERS-CoV. At this time, 13 additional cases with similar symptoms have been recorded. By May 2013, the virus was named the virus that causes Middle East respiratory syndrome (MERS).
From June 2012 to June 30, 2019, there were 2449 confirmed cases of MERS-CoV virus causing Middle East respiratory syndrome and reported to WHO. Of these, up to 84% of cases were recorded in Saudi Arabia. MERS-CoV has spread to 27 countries in the Middle East, North Africa, Europe, Asia and the US. By the time of reporting, there had been a total of 845 deaths from MERS, accounting for 34.5% of infections.
All confirmed cases of MERS-CoV to date have lived or traveled to countries in the Middle East, or been in close contact with infected individuals. MERS-CoV is present in people who have traveled to or lived in Jordan, the United Arab Emirates, Qatar and the United Arab Emirates (UAE).
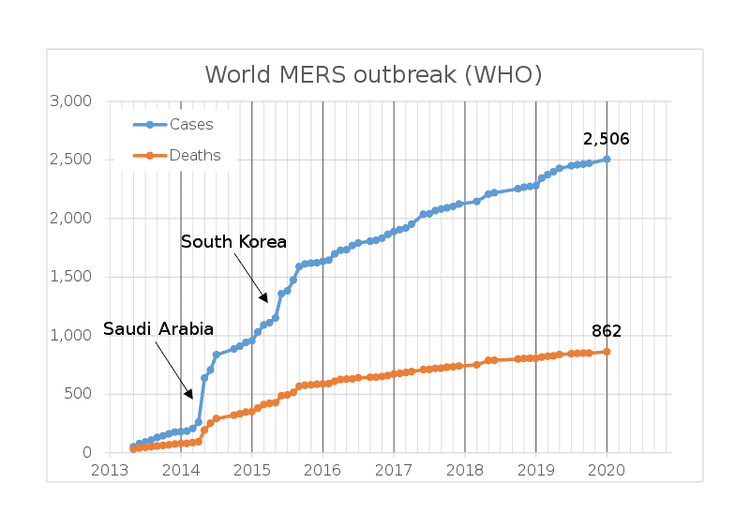
Sơ đồ ghi nhận tốc độ lây nhiễm và tỉ lệ số ca tử vong của dịch MERS năm 2012 (nguồn WHO).
People infected with MERS-CoV virus have also been identified in other countries such as Italy, UK, France, Tunisia, Germany, Kuwait, Oman, Malaysia, Philippines, Egypt, South Korea and Thailand. Some reports of secondary transmission have been reported in countries such as France and the UK from family members or from roommates at the hospital.
The largest outbreak outside the Arabian peninsula occurred in Korea in 2015, which was recorded as a multi-center outbreak. This outbreak has been shown to involve travelers returning from the Arabian peninsula.
As of 30 June 2018, 52 of the 97 secondary cases reported to WHO were related to infection in a health care or healthcare setting. Including 23 cases of medical staff, patients in the same room with MERS patients or patients' family members; however, up to 45 cases of MERS-CoV infection were recorded outside the hospital setting.
New recorded cases include:
February 2019, two regions where MERS-CoV positive patients were detected in Oman, these cases are not related to epidemiological factors, i.e. unspecified. identify the source of infection. Most of these cases were identified as having a familial relationship. The first group in the northern Batinah region includes 9 cases of infection, 2 deaths. Out of these 9 cases, one is a medical worker and has no symptoms. The second group consists of 4 cases, discovered in the southern Sharqia region, including 1 medical worker. Two deaths occurred in this group of patients. In September 2019, 3 cases were detected in Al Qassim locality, in Saudi Arabia, of which 2 cases were fatal and none were medical staff. In addition, there were scattered cases of MERS-CoV infection and death in areas of Saudi Arabia. The most recent on January 9 and 13, 2020, recorded 02 cases tested positive for MERS-CoV. The victims are two men, 51 and 53 years old, who are not medical staff, who have been confirmed positive for MERS-CoV in the United Arab Emirates. According to the WHO report, as of January 15, 2020, the total number of confirmed cases worldwide is 2506 cases with 862 deaths from MERS.
Source: WHO, CDC, PUBMED, CLINIALTRIAL.GOV
MORE:
MERS-CoV: Origin, transmission, recognition and treatment Origin and symptoms of MERS CoV 2019-nCoV are similar to viruses that cause MERS and SARS? Information you need to know about the disease caused by MERS CoV