This is an automatically translated article.
The article was consulted with Specialist Doctor II Tran Thi Linh Chi - Head of Pediatrics - Neonatology - Pediatrics - Neonatology - Vinmec Hai Phong International General Hospital.Neonatal acute respiratory failure is a serious and dangerous disease with a high risk of death. The treatment of patients with acute respiratory failure requires prompt intervention, monitoring, and ongoing care.
1. What is infant respiratory distress syndrome?
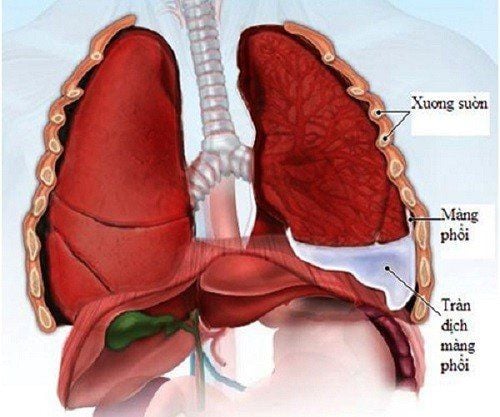
Neonatal acute respiratory distress syndrome (also known as endothelial disease) is a condition when a baby's lungs are still not fully developed after birth, leading to a lack of surfactant (the active ingredient that makes it active) surface), reducing the alveolar surface area available for gas exchange.
This is a very common syndrome in the neonatal period, especially in the first days after birth. Premature infants are more susceptible to respiratory distress than term infants. For babies, healthy lungs are of the utmost importance. Meanwhile, children with acute respiratory failure may have difficulty breathing normally. The number of deaths due to respiratory failure currently ranks first among neonatal deaths, posing a huge problem for the diagnosis of the cause and treatment of neonatal respiratory failure.
2. Causes of acute respiratory distress syndrome in infants
One of the leading causes of acute respiratory distress syndrome in infants is premature birth. The lungs of premature babies often lack surfactant, which is necessary for the expansion and contraction of the lungs. This deficiency is a precursor to shortness of breath and breathing problems. Besides, respiratory failure can also stem from genetic factors related to the child's lung development. In addition to preterm birth, which is considered the main factor, there are a number of other factors that can also lead to acute respiratory distress syndrome in the newborn, including:
Caesarean section Diabetic mother Family history of respiratory failure Maternal multiple pregnancy Perinatal injury: Occurrence of asphyxia and antepartum hemorrhage The blood supply to the fetus during pregnancy is reduced.

3. Symptoms of acute respiratory failure in infants
Most of the symptoms of neonatal acute respiratory distress syndrome can be detected soon after the baby is born. However, some signs may also appear about 24 hours after birth. Common symptoms are:
The child has severe, sudden shortness of breath, then the breathing rate increases rapidly The child's nostrils rise and fall, making a groan when exhaling The phenomenon of pulling on the chest and intercostal muscles, sternum depression Whole body cyanosis, rapid heart rate due to severe lack of oxygen Wheezing due to suffocation Sweating profusely. Although considered a dangerous disease, the symptoms mentioned above are quite similar to those of some other respiratory diseases and infections. Therefore, if the child notices any of the abnormalities listed above, parents should consult a doctor immediately to determine the exact cause and have the right treatment measures.
Patients with acute respiratory failure, if not taken care of in time, this condition can cause the amount of carbon dioxide in the blood to increase, leading to injury to the baby.
4. Complications of acute respiratory failure in infants
Acute respiratory failure in infants can lead to many dangerous complications, long-term effects on the normal development of the child. In some cases, this condition can be life-threatening if not detected and treated promptly. Some complications from acute respiratory failure can include:
Vision loss Blood infections Blood clots formation in the body Mental retardation Accumulation of air around the heart and lungs Brain or lung hemorrhage Dysplasia bronchopneumonia Pneumonia . Severe respiratory failure can also lead to kidney failure and other disorders. Depending on the condition and severity of the disease, the complications encountered in each baby will be different.

5. Diagnosis of acute respiratory failure
5.1. Clinical signs Based on symptoms of labored breathing to assess the severity of the disease, including:
Breathing rate: At rest, fast breathing. Contraction of respiratory muscles in older children is a sign of severe respiratory failure. Unusual breathing sounds: Stridor during inspiration: Signs of laryngeal or tracheal obstruction. Bicycle stridor: Signs of severe laryngeal or tracheal obstruction. Wheezing on expiration and prolonged expiration: Symptoms of lower airway obstruction. Gasping during expiration: Symptoms of respiratory distress are very severe in infants. Auscultating lung sounds dumb: This is a sign of very severe respiratory failure. Alveolar murmur disproportion: Suggesting cause of respiratory failure. Measure SpO2 < 92% without oxygen or SpO2 < 95% with oxygen: Signs of very severe respiratory failure. Based on the consequences of respiratory failure on other organs:
On the cardiovascular system: Sinus tachycardia, paroxysmal tachycardia, arrhythmia, possibly bradycardia, pulse collapse. Blood pressure rises at first to compensate, but if respiratory failure persists or is terminal, blood pressure falls. Cardiac arrest due to severe hypoxia or excessive CO2 may occur. Skin and mucosal condition: Lack of oxygen causes the skin to turn pale due to vasoconstriction. Cyanosis is a late sign. Central cyanosis: Indicates that the baby is about to stop breathing. Sweating profusely. Consciousness: The child is agitated, lethargic, comatose, decreased muscle tone. Signs in other organs such as: liver, biliary tract, urinary kidney. 5.2. Subclinical signs Arterial blood gas is a sign that helps in diagnosing and distinguishing the type of respiratory failure, assessing the severity of the disease and the impact of acute respiratory failure on metabolism. thereby helping guide the treatment and management of acute respiratory failure. Arterial blood gas changes in neonatal acute respiratory distress syndrome: PaO2 index < 60 mmHg, SaO2 < 92% and/or PaCO2 > 50 mmHg Need to see the value of pH, bicarbonate, residual alkali. Chest X-ray: Should be indicated for all patients with acute respiratory failure, in order to detect the cause of the disease and distinguish the type of respiratory failure with damage to the lungs, from which to have a treatment. best fit. Blood biochemical tests: There are accompanying biochemical disorders, commonly increased potassium, decreased blood calcium. Complete blood count: white blood cells, hemoglobin, platelets. Microbiological tests: Flu test, nasopharyngeal culture culture, endotracheal fluid analysis...

6. Treatment of neonatal respiratory failure
6.1. Quickly bring O2 and CO2 in the blood to normal. Patients with acute respiratory failure need to have their airways cleared: Put in the correct position, aspirate nasopharyngeal fluid and provide oxygen.
Indications for oxygen breathing in the following cases:
The child has cyanosis and/or SaO2 < 92% and/or PaO2 < 60 mmHg The child has signs of severe chest contraction, rapid breathing over 70 times/minute. Methods of providing oxygen to the baby:
Normal oxygen delivery method: Nasal oxygen (flow 0.5 - 3 liters / min), oxygen mask (flow 6 - 8 liters / min) or breathing oxygen through a hat Plastic (Hood) (flow 5-8 liters/min) Advanced oxygen delivery method: Applied when patients with acute respiratory failure use normal oxygen breathing method but have rapid breathing, severe respiratory muscle contraction , pale skin, SpO2 decreased < 92% and or PaO2 < 60mmHg. At this time, give the baby oxygen through a mask with a reserve bag of 6 - 10 liters/min for re-breathing masks (FiO2 60 - 80%) and non-rebreathing masks (FiO2 60 - 100%), continuous positive pressure breathing. nasal passage (NCPAP). It also applies when intubation and mechanical ventilation fail with O2 through a mask or when the patient is unable to breathe on his own. 6.2. Enhance the effect of the O2 transport system Ensure optimal hemoglobin concentration (> 100g/l): Transfuse red blood cells... Ensure stable cardiac output: Give fluids to support preload, Adjust if there is electrolyte disturbance, use inotropic drugs, raise blood pressure, treat arrhythmia if present. Provide adequate oxygen in the tissues: Avoid hypothermia, alkalosis (when metabolic acidosis, appropriate sodium bicarbonate should be given based on blood gas results) Reduce unnecessary oxygen consumption: Treat when fever is present, avoid stimulate. 6.3. Facilitating the repair and healing of lung damage Limiting the occurrence of oxygen poisoning: Breathing oxygen correctly indicated, method, dose and time. Ensure adequate nutrition: Should give the child oral food, if the child cannot eat, put a nasogastric tube, pump milk on an hourly basis or drop a basket into the stomach. Energy needs to increase by 30% to 50% compared to normal needs due to rapid breathing. Prevention of the risk of superinfection and nosocomial infection: The care and treatment of neonatal respiratory failure must ensure aseptic, especially when performing endotracheal aspiration sputum. Prescribe appropriate antibiotics according to the results of the antibiogram. Perform specific intervention if there is mechanical obstruction: Remove airway foreign body, puncture or drain fluid, pneumothorax, use bronchodilator. 6.4. Transport the child in acute respiratory distress Clear the airway Place in a safe position Provide adequate oxygen Maintain body temperature Prevent hypoglycaemia.
7. Prevention of acute respiratory failure in infants
The main cause of acute respiratory distress syndrome in infants is premature birth. Therefore, to prevent the disease, the best way is for pregnant women to try to have a full-term baby, reduce the risk of premature birth by maintaining good habits, avoiding bad effects, such as not drinking alcohol, smoking during pregnancy.
In the event that an early delivery is required, the doctor may prescribe the pregnant woman to take medicine to make the baby's lungs grow faster, to increase the production of active substances, to create the surface surface of the baby's lungs, prevent acute respiratory failure.
Treatment of acute respiratory distress syndrome in infants is considered a great challenge because this condition requires the baby to be monitored and cared for continuously with appropriate and correct methods. Besides, early hospitalization time is also a decisive factor for success in treatment.
Indications Surfactant pump is applied in the treatment of respiratory failure in premature infants. In the past, medicine often used the technique of endotracheal intubation with surfactant and mechanical ventilation for children. Currently, surfactant pump technique for treatment of neonatal respiratory failure is less invasive and is increasingly widely used. If the child is found to have respiratory failure, surfactant should be used for early treatment.
Clinical benefits of Surfactant therapy include: Improved lung ventilation; Enhance blood oxygenation; Reducing the frequency of air leaks (complications with pneumothorax, alveolar retention...); Reducing child mortality and morbidity; Reducing the rate of severe disability...
Surfactant pump technique in the treatment of respiratory failure in infants has been independently deployed at Vinmec Hai Phong and Nha Trang International General Hospitals since April 2019.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.