This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Van Phan - Head of Interventional Imaging Unit - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International General Hospital. Doctor Nguyen Van Phan is an interventional radiologist and radiologist.Pancreatic duodenal artery intervention is essentially embolization techniques to block the circulation of blood vessels in the vessel lumen. Indications for implementation are in pathologies with gastrointestinal bleeding. By using the catheter, microcatheter super-selective into the arterial branches to cause bleeding and block these branches to stop the bleeding, the patient's condition will rapidly improve.
1. What is pancreaticoduodenal vascular intervention?
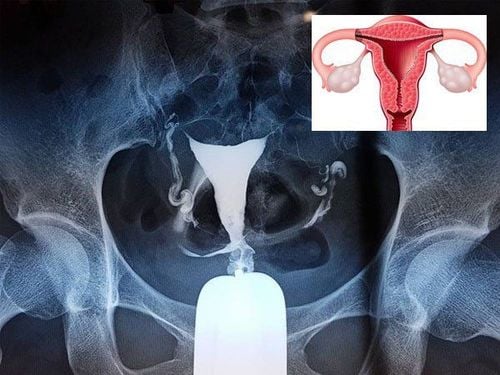
The pancreaticoduodenal artery is a branch of the gastric artery, usually arising from the common hepatic artery from the celiac artery. The pancreatic duodenal artery divides into two branches as it descends, one anterior and one posterior. Each branch is further divided into two parts, the upper part and the lower part.The superior parts of the anterior and posterior branches move around the head of the pancreas and duodenum, eventually joining the anterior and posterior branches of the inferior pancreaticoduodenal artery. The inferior pancreatic artery is also considered a small branch of the superior mesenteric artery. These arteries, together with the pancreatic branches of the splenic artery, form interconnected arterial rings, allowing blood to perfuse the pancreas and duodenum through multiple channels.
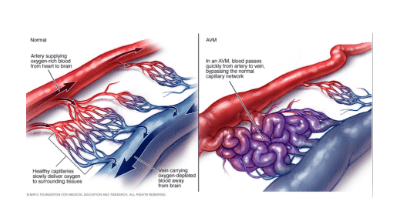
When one of these branches is damaged by any pathology, the vessel wall loses its stability, the blood vessel ruptures and bleeds into the abdomen. Risks may be secondary to infection, trauma, or pancreatitis, or may be primary to aneurysms. Because it is located deep in the abdomen, under the pressure of blood supply from the visceral artery, which is an important branch from the abdominal aorta, the amount of blood that flows from the rupture site has a relatively large volume and the disease state The patient quickly becomes critical if not intervened early.
However, because this visceral region is located deep in the abdomen, laparotomy is difficult while the patient is hemodynamically unstable. In this context, pancreaticoduodenal vascular intervention is considered to be the optimal measure, minimally invasive, fast implementation time, but the efficiency is quite high.
Indications for digitized angiography and pancreatic duodenal angiography commonly used in clinical practice are:
Pseudoaneurysmization after liver and biliary tract infection Pseudoaneurysmal aneurysm after acute pancreatitis, gastric ulcer thick - duodenum Pseudoaneurysmectomy after interventional procedure: drainage - placement of biliary support brackets, percutaneous abdominal drainage, endoscopic resection of Oddi... Closed abdominal trauma with vascular injury causing Abdominal bleeding Aneurysms, pseudoaneurysms Arteriovenous malformations.
2. Process of digital scan to erase the background and intervene in pancreatic duodenal vessels
Patients and relatives need to be thoroughly explained about the procedure to be prepared, as well as the risks involved, in order to ask for cooperation. Next, the patient needs to fast or not fast because in an emergency situation, change into appropriate clothes and arrange to lie on his back on the intervention table, place an intravenous line with physiological saline solution 0. 9%. Means of monitoring breathing, pulse, blood pressure, electrocardiogram, SpO2 are mounted on the patient and the indicators are displayed on the screen for easy observation. After cleaning the inguinal area on both sides, the doctor will cover the area with a sterile tissue to prepare for intervention. In case the patient is overstimulated and poorly cooperated, it is necessary to consider appointing a sedative to facilitate the procedure; however, the adverse effect of sedation on hemodynamic status should be borne in mind.At the intervention site, the doctor will administer local anesthesia. The site chosen was from the right common femoral artery. Once the anesthetic has worked, the doctor will insert a needle and place an arteriostat into the right femoral artery. Next, the lead and catheter will also be threaded into the lumen, inserted into the visceral trunk artery and pancreatic duodenal artery. In order to determine the exact location of the lesion and the extent of the arterial tear, the doctor will use a volume of contrast agent injected into the blood vessel, the entire vascular system supplying the duodenum and pancreas will be clearly visible. At this point, a microcatheter will approach and selectively take DSA of the affected artery.
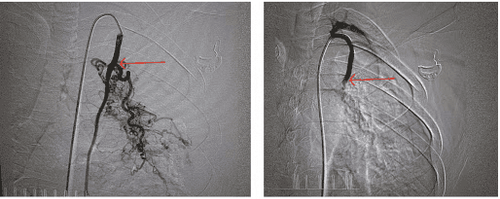
The features of the pancreatic duodenal vasculature will be fully assessed quickly. The doctor will use a microcatheter to selectively approach the damaged artery branch and conduct embolization with suitable materials, which can be metal coils or bio-glue. When these materials are injected into the vessel lumen, the blood vessel will be blocked, and the bleeding will stop.
However, before concluding, the doctor needs to evaluate the post-intervention by taking a picture of the arterial system supplying the pancreatic duodenum again. Under the background digitized angiogram screen, the arterial branches and collaterals circulate normally, without thrombus. At the same time, the doctor will also evaluate the most focused assessment is that the bleeding site has been completely blocked by intervention, no longer communicates with the pancreatic duodenal artery system or no longer leaks contrast material outside the lumen into the artery. Abdominal.
For the case of pseudoaneurysm node intervention, the pseudoaneurysm should be determined to have been completely removed from the pancreatic duodenal artery circulation while the circulation around the pseudoaneurysm is normal. In addition, the preliminary ultrasound examination also did not show hematoma around the liver and abdomen.
When the above requirements have been met, this procedure will end. The doctor will pull out all the catheters, microcatheters, and wires. The puncture artery site will be directly pressed by hand for about 15 minutes to stop bleeding and then bandaged for 8 hours. During this time, the patient is limited to bed movement.

3. Complications that may be encountered in digital scan and pancreaticoduodenal vascular intervention
As with any endovascular procedure, digital angiography and pancreaticoduodenal angiography may also carry certain risks, especially when the pancreatic duodenal vasculature is often small in size and Located deep in the internal organs, the collateral circulation is quite rich and diverse in anatomical details.Accordingly, complications that may be encountered in digital angiography and pancreaticoduodenal vascular intervention include:
Necrotizing enterocolitis due to thrombus formation, blocking the branch of the artery supplying the intestine; Dynamic tearing vessels causing abdominal bleeding Arterial dissection Hematoma or bleeding at the femoral puncture site Infection at the femoral puncture site Complications related to anesthesia, anesthesia, or the use of contrast agents.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.