This is an automatically translated article.
The article was written by Specialist Doctor I Nguyen Thi Minh Thuyen - Pathologist, Pathology Department - Vinmec Danang International General Hospital.The pathological diagnosis of multiple myeloma on biopsy tissue is difficult and complicated because the lesions are very diverse, it is necessary to combine the histopathological images and enough immunohistochemical markers to diagnose the lesion morphology. , plasmacytoplasmic ratio and morphology, the percentage of plasma cells in bone marrow as well as determination of malignant plasma cells or activated plasma cells.
1. Diagnosis of multiple myeloma
Multiple myeloma is usually diagnosed based on laboratory tests, patient symptoms, and physical examination. The diagnosis of multiple myeloma requires BOTH of the following:
A tumor of plasma cells (confirmed by biopsy) OR at least 10% of plasma cells in the bone marrow and at least one of the following conditions:
High blood calcium levels Poor kidney function Low red blood cell count (anemia) An image of a cavity in the bone from a tumor as determined by imaging tests (X-ray, CT, MRI, PET scan) Yes >= 60% plasma cells in bone marrow

Histopathological diagnosis is based on tissue biopsy:
The histopathologic pattern of multiple myeloma is very diverse: there may be one or more lesions on the same biopsy slide: diffuse, tissue interstitial, nodular, clustered, and mixed.
● Diffuse pattern: plasma cells gather in large clumps, spread to the entire medullary cavity, the percentage of normal blood cells (red blood cells, white blood cells, platelets) is very little.
● Interstitial pattern: plasma cells are scattered among normal hematopoietic cells, the number of plasma cells is not more than that of normal hematopoietic cells.
Nodal pattern: plasma cells aggregate into nodal nodules, located in the medullary cavity (very few normal hematopoietic cells in the plasma nodule), do not occupy all the medullary sinuses, and around the nodule. no or very few plasma cells.
● Small cluster pattern: aggregation of a few plasma cells in small clusters in the medullary cavity between normal hematopoietic cells
● Mixed morphology: possibly diffuse-interstitial; nodules-interstitial tissue; diffuse-nodular; a collection of plasma cells that confer the morphology of one form at one site and the other at another site on the same biopsy specimen
2.Staging and Prognosis
After a patient is diagnosed with cancer, doctors try to find out if it has spread, and if so, how far. This process is called staging. It helps determine the severity of the cancer and the best treatment. Doctors also use cancer stage when talking about survival statistics.
2.1 Staging systems International staging system (ISS)
This system (ISS) is now commonly used to classify multiple myeloma. The ISS is based on data collected from people with multiple myeloma from around the world. The system is divided into three phases based on measurement of albumin and serum β2-Microglobulin levels.
● Stage I:
- β2-Microglobulin blood <3.5 mg/L
AND
- Albumin blood >= 3.5 g/dL
Stage II:
- β2-Microglobulin: 3.5 mg/L - 5 ,5 mg/dL
AND/OR
- Albumin <3.5 g/dL
● Stage III:
- β2-Microglobulin > 5.5 mg/L

2.2 The Revised International Staging System (R-ISS) The ISS system has recently been modified to the Revised International Staging System (R-ISS).
This system diagnoses multiple myeloma based on 4 factors:
Serum albumin amount Serum β2-Microglobulin Serum LDH amount Cancer-specific genetic abnormalities (cytogenetics) ● Stage I
- Beta-2 microglobulin blood < 3.5 (mg/L)
AND
Albumin >= 3.5 (g/dL) AND
“Non-high risk” cytogenetics AND
normal LDH
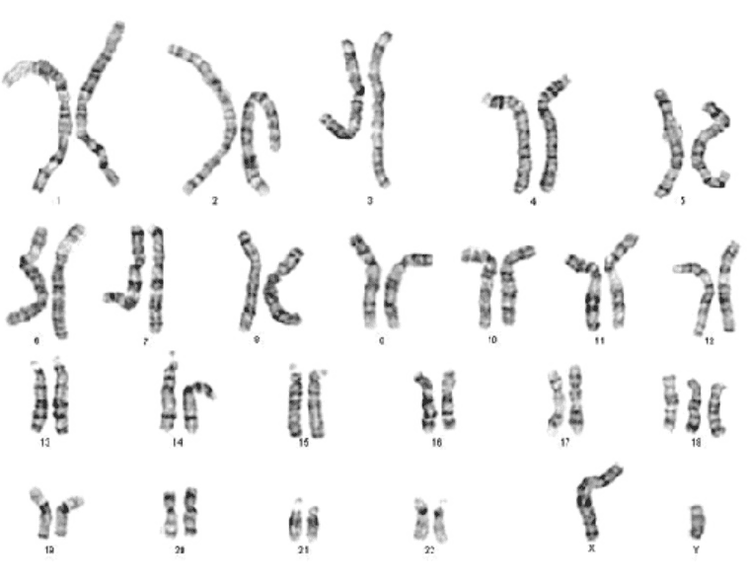
Stage II
Not in stage I or III
● Stage III
- Beta-2 microglobulin >= 5.5 (mg/L)
AND
“high-risk” cytogenetics AND/OR
High LDH ▫ Cytogenetics: a bone marrow test to look for chromosomes in cancer cells is also known as cytogenetics. Certain chromosomal changes may have a worse prognosis.
✓The “high-risk” group has the following changes:
Loss of a chromosome segment 17 Translocations of chromosomes 4 and 14 Translocations of chromosomes 14 and 16 ✓The group is “moderate risk” or “ not high risk” have other chromosomal abnormalities
Cancer staging can be complicated, so ask your doctor to explain it to you in a way you can understand.
3. Recurrent multiple myeloma
The disease that comes back after a period of control after treatment is called recurrent multiple myeloma. If there is a recurrence, the cancer may need to be re-staged using one of the systems above.
3.1 Prognosis Other factors that affect survival include:
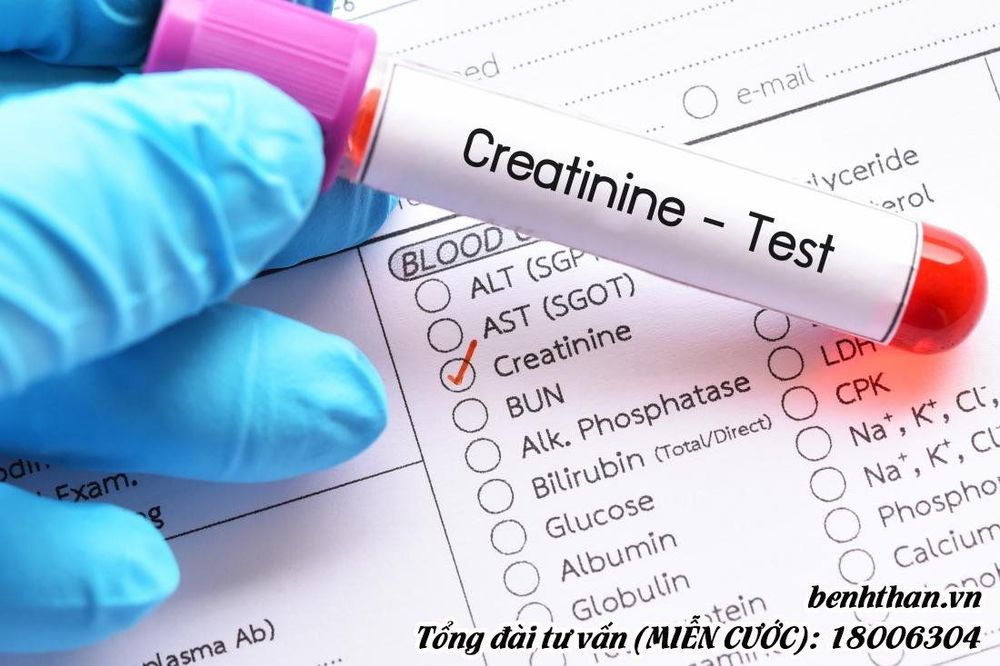
✓ Kidney function
The level of creatinine in the blood indicates how well the kidney functions. The kidneys remove this chemical from the body. When they are destroyed by monoclonal immunoglobulin, blood creatinine levels increase, predicting a worse prognosis.
✓ Age
Age is also important. In studies of the international staging system, elderly people with myeloma do not live long.
✓ General health
Overall health can affect the prognosis of someone with myeloma. Poorly controlled health, such as diabetes or heart disease, may have a worse prognosis.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article referenced source: American Cancer Society