This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
The most common atypical presentation of GERD may include ear, nose, and throat (ENT) symptoms, pulmonary (chronic cough or asthma), or cardiac symptoms (noncardiac chest pain). Therefore, GERD should be strongly considered in the differential diagnosis of patients with atypical symptoms when alternative diagnoses have been ruled out by another specialist (ear, nose and throat surgeon, physician) Cardiologist, Respiratory Physician, Allergist).
1. Empiric therapy
In patients with a history suggestive of uncomplicated GERD presenting with typical symptoms of heartburn and/or regurgitation may be treated empiric. Typical symptoms in response to acid suppression provide further evidence for pathological esophageal acidosis and it is reasonable to assume the diagnosis of GERD in patients who respond to appropriate therapy. On the other hand, typical symptoms that do not improve require further testing to demonstrate the existence of GERD and evaluation for an alternative diagnosis. Similarly, patients with atypical presentation or noncardiac chest pain should be considered for esophageal function testing prior to empiric therapy.
However, this empiric test is contraindicated in patients with alarming symptoms such as dysphagia, weight loss, and bleeding according to the five recommendations of the Italian Association of Hospital Gastroenterologists (AIGO).
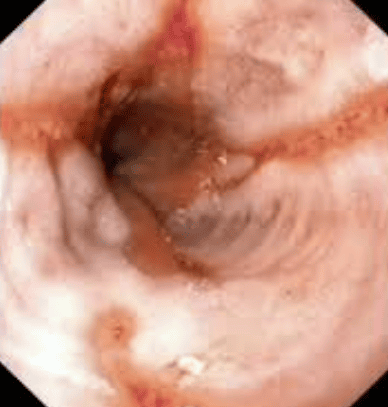
2. Upper gastrointestinal endoscopy
Upper gastrointestinal endoscopy allows evaluation of the esophageal mucosa in GERD patients and biopsy samples of associated lesions (eg, Barrett's metaplasia, esophageal stricture or tumor). There are limitations to the use of upper endoscopy in the diagnosis of GERD. Erosive reflux disease (ERD) occurs in a small number of patients with GERD (<30%), whereas the majority of them are included in the non-erosive reflux disease (NERD) phenotype, which is characterized Because of typical reflux symptoms, mainly heartburn, no esophageal mucosal lesions were visible on upper gastrointestinal endoscopy. Patients with atypical GERD symptoms often have a low incidence of endoscopic esophagitis. Therefore, upper gastrointestinal endoscopy is not diagnostic and is mainly performed to evaluate GERD-related complications and alternative diagnoses. Patients with alarming symptoms, such as anemia, weight loss and dysphagia, or a history of chronic GERD, and who are 50 years of age or older should have Barrett's esophagus endoscopically.
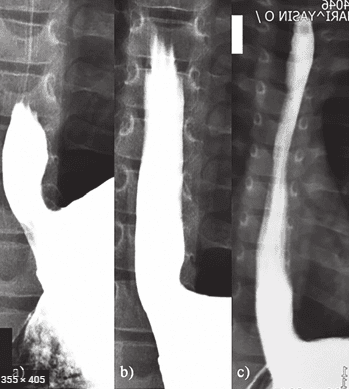
3. Contrast X-ray with Baryt Contrast
Baryt radiographs have historically been considered part of a potential diagnostic approach in patients with esophageal symptoms, including GERD. Although well-performed Baryt esophagography with dual contrast can detect signs of esophagitis, the overall sensitivity of this test is extremely low. The detection of reflux with Baryt contrast above the thoracic entry with or without provocative manipulations including water siphon testing increases the sensitivity of the Baryt contrast test; however, is not sufficient to be recommended as a diagnostic test without dysphagia.
4. Esophageal pressure measurement
Esophageal manometry is now considered the gold standard test for diagnosing esophageal dysfunction that can cause symptoms such as difficulty swallowing and chest pain. However, it has shown limited ability to diagnose GERD. With the advent of high-resolution manometers, it is now possible to more accurately assess esophageal motility. Furthermore, new measures have been developed to investigate the morphology and function of the gastroesophageal junction (EGJ). In particular, the antireflux barrier function of the gastroesophageal junction can now be assessed by evaluating the contractility integral of the junction. In addition, transient lower esophageal sphincter dilation can be more accurately identified with high-resolution manometry. Neither a decrease in lower esophageal sphincter pressure nor the presence of a motility abnormality are specific enough to diagnose GERD.
5. Measure Bilirubin concentration in 24 hours
Bilimeter allows spectral measurement of bilirubin levels in the esophagus due to gastroduodenal reflux (gastroduodenal reflux).
Although the role of bile in the pathogenesis of esophageal mucosal injury is unknown and there is a high prevalence of both acid and non-acid reflux, some authors recommend simultaneous monitoring of pH and measure billan.
The main indications for dual monitoring are patients with typical GERD symptoms who respond poorly to PPI therapy.
Bilitec 2000 is a new spectrophotometer system. Unfortunately, this technology is only a semi-quantitative measure for the detection of GERD. Validation studies show that this device underestimates bile reflux in acidic environments (pH <3.5). In solutions with pH <3.5, bilirubin undergoes monomer isomerization to dimer as reflected by a change in absorption wavelength from 435 nm to 400 nm. Since the Bilitec reading is based on absorption detection at 470 nm, this variation underestimates the extent of GERD. Therefore, Bilitec measurements of GERD should always be accompanied by simultaneous measurements of acid exposure by pH monitoring. Furthermore, many substances can cause false-positive results by Biltec, as it indiscriminately records any substances absorbed around 470 nm such as heme (i.e. during emesis), porphyrins, carotenoids , riboflavin and various foods such as tomatoes, bananas, carrots, beets, parmesan, cheeses, meat, tea and coffee. In addition, solid food can interfere with the transducer and reduce the accuracy of the records, for these reasons a standardized liquid diet is recommended to allow for registration. However, there was a limitation in the registration of gastroduodenal reflux patterns due to a different and lower calorie diet.
Although the measurement of bilirubin adds valuable information about the chemical nature of the flowing material, there are a number of limitations that do not allow for accurate and precise detection of the onset and frequency of flushes. gastroduodenal reverse.
Vinmec International General Hospital examines and treats gastroesophageal reflux disease with the most optimal internal - surgical methods for patients, both children and adults. Coming to Vinmec International General Hospital, patients will receive direct, dedicated and professional examination from a team of qualified and experienced medical staff.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesCesario Silvia,1 Scida Serena, et al., Diagnosis of GERD in typical and atypical expressions, Acta Biomed. 2018; 89(Suppl 8): 33–39. El-Serag Hashem B, et al. “Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review” Gut. 2013 gutjnl-2012. [PMC free article] [PubMed] [Google Scholar] Vakil Nimish, et al. “The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus” The American journal of gastroenterology. 2006;101(8):1900. [PubMed] [Google Scholar]4. Vaezi Michael F. “Atypical expressions of gastroesophageal reflux disease” Medscape General Medicine. 2005;7(4):25. [PMC free article] [PubMed] [Google Scholar]5. Lacy Brian E, et al. “The diagnosis of gastroesophageal reflux disease” The American journal of medicine. 2010;123(7):583–592. [PubMed] [Google Scholar]6. Aanen M.C, et al. “Diagnostic value of the proton pump inhibitor test for gastro-oesophageal reflux disease in primary care” Alimentary pharmacology & therapeutics. 2006;24(9):13771384. [PubMed] [Google Scholar]














