This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalEosinophilic gastroenteritis (English used from Eosinophilic gastroenteritis_EG) is a disease in the following group of diseases: eosinophilic esophagitis (eosinophilic esophagitis), gastritis, enteritis, colitis eosinophil gastritis, enteritis, and colitis), and members of this family of diseases are collectively known as eosinophilic gastrointestinal disorders (EGIDs).
1. Diagnosing eosinophilic gastroenteritis
Although rare, eosinophilic gastroenteritis should be recognized by the clinician as soon as possible because the disease presents with signs, symptoms, and syndromes that are "similar" to some other diseases. Other digestive diseases, especially peptic ulcers, but still not cured with proper treatment. Furthermore, eosinophilic gastroenteritis is treatable, sometimes presenting as masquerade as the irritable bowel syndrome.
This is a diagnosis based mainly on histopathology with an increase in BCAT count in biopsies of gastrointestinal mucosa and exclusion of causes of local elevation of BCAT. However, the criteria for histopathology to date have not been agreed, so the role of the pathologist in conjunction with the clinician is very important. The diagnosis of EG is confirmed by biopsy or collection of eosinophilic ascites in the absence of other pathogens, including intestinal parasites. Eosinophilic esophagitis should also be differentially diagnosed and discussed.
2. Subclinical in eosinophilic gastroenteritis
2.1. Testing After taking a thorough history and physical examination, it is necessary to look for specific food and environmental factors that can trigger allergies and manifestations of allergic diseases such as asthma, allergic rhinitis, and allergic rhinitis. sinuses. Tests indicated when eosinophilic gastroenteritis is suspected include:
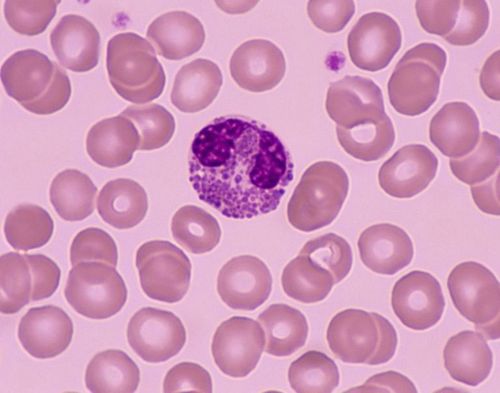
Blood count in which peripheral eosinophil count (BCAT) > 600 cells/HL is of a nature suggestive of elevated BCAT. The degree of peripheral eosinophilia is divided into three categories: mild (600 - 1500 cells/BL), moderate (1500 - 5000 cells/ML) and severe (> 5000 cells/ML). The prevalence of elevated BCAT in the peripheral blood of patients with eosinophilic gastroenteritis ranges from 20 to 80%. Elevated erythrocyte sedimentation rate, iron deficiency anemia, increased IgE levels, and low blood albumin can be seen. Stool tests to rule out parasitic infections, c-1 antitrypsin tests, and fecal fat should be performed.

Evaluation of allergies by skin prick tests, skin prick tests to find out the type of food or allergens in the specific environment to help find the triggering factors for the occurrence and progression of symptoms. However, during the study of the pathogenesis of eosinophilic gastroenteritis, there was a combination of IgE- and non-IgE-mediated responses when epithelial cells gastrointestinal tract exposed to allergens. In addition, each person's body has adaptations to increase tolerance for allergens. Therefore, although it is possible to use allergy tests to find out specific allergen factors, it cannot be based on this result alone to diagnose inflammatory gastrointestinal diseases caused by BCAT.
2.3. Imaging methods The application of imaging methods in this pathology is limited because the imaging features are often nonspecific.
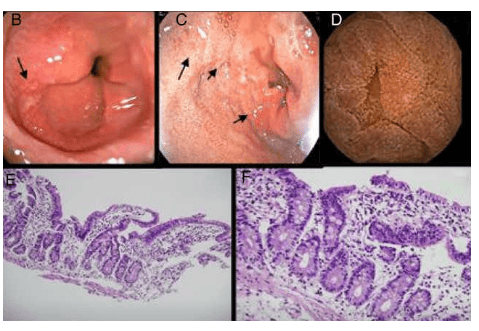
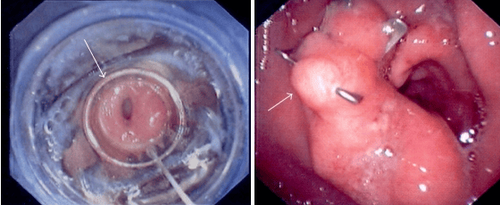
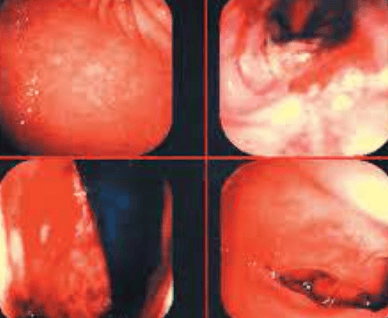
Ultrasound: With the advantage of being a non-invasive procedure, low cost, available in many units, ultrasound can detect cases of eosinophilic gastroenteritis with thick intestinal wall or abdominal fluid. This method can be used to monitor a patient's response to treatment. Computed tomography of the abdomen can show thickening of the gastrointestinal wall, abnormal folds, and peritoneal fluid. In patients with BCAT-associated colitis, colonic thickening, particularly in the cecum region, may also be seen in the terminal ileum, with mild to moderate thickening. This image is sometimes easily confused with Crohn's. Baryt scan can show images of pylorus narrowing, abnormal gastric mucosa, thickening of small intestinal mucosal folds due to edema... 2.4. Endoscopy The endoscopic appearance of eosinophilic gastroenteritis may be normal or have nonspecific inflammatory lesions including mucosal edema, mucosal bleeding, mucosal roughness or mild papules. In addition, in the stomach can see images of ulcers, thickening of mucosal folds.
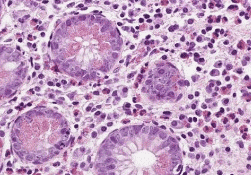
2.5. Histopathology Confirmation of the diagnosis of eosinophilic gastroenteritis must be based on histopathological findings of biopsies taken from the stomach, small intestine (usually duodenum), colon, or rectum. Among the segments of the gastrointestinal tract, the cecum and the appendix are the sites with the highest BCAT counts (up to 30 cells/microfield). The stomach and colon have lower BCAT counts, so the standard for diagnosing eosinophilic gastroenteritis in most studies is when the BCAT count is above 20 cells/microfield. The distribution of BCAT is characterized by regional characteristics, so multiple biopsies including normal mucosal areas help confirm the diagnosis. Using immunohistochemical staining methods also helps determine the deposition of substances released from extracellularly deposited BCAT particles such as MBP, ЕСР. . In the case of musculoskeletal or serosarcoma VDDRDBCAT, it may be necessary to combine with laparoscopy or capsule endoscopy to obtain specimens to confirm the diagnosis.
3. Conclusion
To date, there is no consensus or specific guideline on the diagnostic approach in eosinophilic gastroenteritis. Therefore, clinically suspicious cases should be taken with multiple biopsies (4-5 pieces/site) from the gastric mucosa or colon for confirmation. In addition, careful history taking, combined laboratory results, imaging studies and endoscopy help rule out other possible causes of increased BCAT in the gastrointestinal tract.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic and treatment techniques for digestive diseases. Along with that, at Vinmec Hospital, the diagnosis of gastrointestinal diseases is done through gastroscopy and colonoscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging - endoscopy) function. endoscopic examination with narrow light spectrum) results in clearer mucosal pathological analysis results than conventional endoscopy, detecting inflammatory lesions, early gastrointestinal cancer lesions. Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can rest assured with the gastrointestinal endoscopy service at the hospital. Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References 1. Kaijser R (1937). Allergic diseases of the gut from the point of view of the surgeon. Arch Klin Chir, 188.36-64. 2. Ureles A. L., Alschibaja T., Lodico D. et al (1961). Idiopathic eosinophilic infiltration of the gastrointestinal tract, diffuse and circumscribed; a proposed classification and review of the literature, with two additional cases. Am J Med, 30,899-909. 3. Klein N. C., Hargrove R. L., Sleisenger M. H. et al (1970). Eosinophilic gastroenteritis. Medicine (Baltimore), 49(4), 299-319. 4. Oyaizu N., Uemura Y., Izumi H, et al (1985). Eosinophilic gastroenteritis. Immunohistochemical evidence for IgE mast cell-mediated allergy. Acta Pathol Jpn, 35(3), 759-766. 5. Naylor A. R. (1990). Eosinophilic gastroenteritis. Scott Med J, 35(6), 163-165. 6. Lee C. M., Changchien C. S., Chen P. C. et al (1993). Eosinophilic gastroenteritis: 10 years experience. Am J Gastroenterol, 88(1), 70-74. 7. Uppal V., Kreiger P., and Kutsch E. (2016). Eosinophilic Gastroenteritis and Colitis: a Comprehensive Review. Clin Rev Allergy Immunol, 50(2), 175-188