This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Hemorrhagic ulcerative colitis is a chronic inflammatory disease causing continuous inflammation of the colonic mucosa with histopathological characteristic of granulomatous lesions. If the disease progresses seriously, it is necessary to have accurate diagnosis methods and timely treatment to avoid bad consequences.
1. Diagnosis of bleeding ulcerative colitis
1.1. Implementing the quadrants
Definitive diagnosis of bleeding ulcerative colitis is based on many factors including clinical symptoms, laboratory tests, endoscopic imaging features and histopathology:
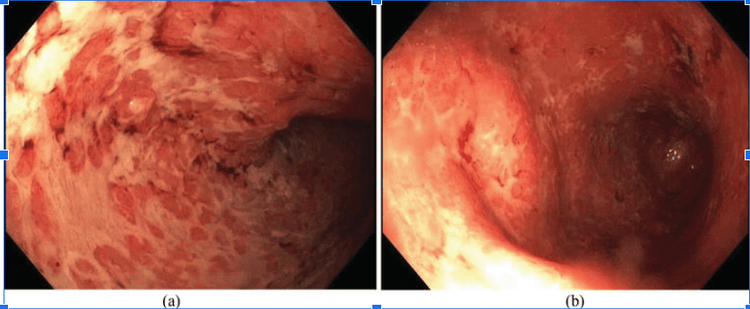
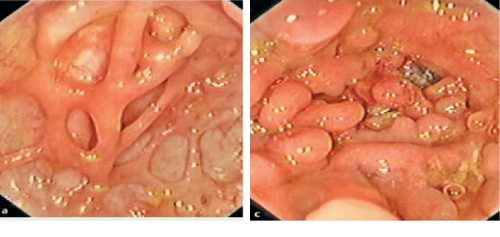
Clinical symptoms (symptoms appear at least 4 weeks): Diarrhea, small or large amount of blood in the stool, abdominal pain during or around the time of defecation. Gastrointestinal tract infections should be excluded. Laboratory tests: Iron deficiency anemia, thrombocytosis, hypoalbuminemia, autoantibodies (DANCA), increased fecal calprotectin. Features of colonoscopy imaging: Diffuse inflammatory lesions are typical in the rectum, then gradually spread to the upper segments of the colon with features such as loss of capillary network, loss of colonic folds. , mucosal edema, congestion, exudation, many ulcers, ulcers on the surface, easy bleeding when inflated or touched with lights, real bleeding. In cases of chronic inflammation for a long time, a pseudo-polyp may be seen. Histopathological features: Increased infiltration of monocytes in the epithelial connective membrane, disappearance of mucin-secreting goblet cells, distorted glandular slits, branching, atrophy, microabscesses in glandular clefts .
1.2. Level diagnosis
Bleeding ulcerative colitis can be classified according to types based on location, severity, age of onset and extra-gastrointestinal manifestations. Among them, the Montreal classification that assesses both location and severity is most commonly applied.
Plasma cell infiltration in the basement membrane: This is an early diagnostic sign with high predictive value and helps in the differential diagnosis between bleeding ulcerative colitis (61%) and infectious colitis (6%). ). This feature can be seen in 38% of ulcerative colitis patients bleeding within 2 weeks of symptom onset. Other features indicative of chronic inflammation: Paneth cell metaplasia (especially in left-sided colitis), inflammatory polyps, muscularis hyperplasia, and sometimes severe, chronic inflammatory cases can see fibrosis in the submucosal layer but the rate is very low. The image of granulomas is not seen in bleeding ulcerative colitis.
Evaluation of severity of ulcerative colitis according to the Montreal classification
| Thuật ngữ | Mức độ | Mô tả |
| S0 | Hồi phục | Không có triệu chứng |
| S1 | Nhẹ | Đi ngoài ít hơn hoặc bằng 4 lần/ngày, có thể có máu, không có triệu chứng toàn thân, chỉ số viêm bình thường |
| S2 | Trung bình | Đi ngoài 4 lần/ngày, triệu chứng toàn thân ít |
| S3 | Nặng | Đi ngoài >6 lần/ngày, có máu, mạch >90 lần/phút, nhiệt độ 237,5ºC, Hb < 105 g/l, tốc độ máu lắng > 30 mm/giờ. |
2. Differential diagnosis
The table below summarizes the common differential diagnoses of ulcerative colitis, which are divided into three main groups: inflammatory bowel disease, infectious and non-infectious causes. Differential diagnosis of bleeding ulcerative colitis| Nhóm nguyên nhân | Các bệnh lý cụ thể |
| Bệnh lý IBD khác | Crohn, viêm đại tràng không xác định thể |
| Nguyên nhân nhiễm trùng | Clostridium difficile, Salmonella, Shigella, E.coli, Campylobacter jejuni, Entamoeba histolytica, Cytomegalovirus |
| Nguyên nhân không nhiễm trùng | Viêm đại tràng thiếu máu, viêm đại tràng do xạ trị, bệnh Behcet, viêm đại tràng vì thế, viêm đại tràng do thuốc hoặc nhiễm độc, loét đơn độc ở trực tràng, viêm đại tràng do thâm nhiễm bạch cầu ái toan |
Take a thorough medical history, history, especially travel history, food intolerances, medications used and family history as well as the initial clinical examination plays an important role in orientation. . The differential diagnosis of Crohn's has been covered individually in the previous sections including clinical, endoscopic imaging, and histopathology. Approximately 10% of patients with chronic colitis who do not meet the criteria for a diagnosis of Crohn's or hemorrhagic ulcerative colitis are classified as unclassified. The combination of additional serological markers or capsule endoscopy will help to make a clear diagnosis of 50% of patients in this group. Among the infectious etiologies, the most common microorganisms causing acute colitis are Salmonella, Shigella and Campylobacter jejuni. The general symptoms of this group of diseases include fever, abdominal pain, vomiting/nausea. In addition, when infected with Shigella, one of the typical symptoms is bloody stools. Pre-use of antibiotic classes is a suggestion to target C.difficile pseudomembranous colitis.
In the group of non-infectious causes, ischemic colitis may occur in patients with certain underlying conditions such as Henoch-Scholein, Churg-Strauss syndrome, and Wegener's disease. Up to 6-13% of patients with Behcet have gastrointestinal manifestations and are difficult to distinguish from IBD. Microscopic colitis consists of lymphoid and collagenous bodies with clinical symptoms including chronic, watery, severe and non-bloody diarrhea. The differential diagnosis is mainly based on histopathology. In addition, many drugs cause ulcerative lesions and anemia in the colon, in which NSAIDs can cause symptoms of abdominal pain and bloody stools.
3. Principles of treatment and assessment of treatment response
The choice of treatment modality depends on the severity and extent of the lesion and the individual characteristics of each patient such as frequency of recurrence, disease course, response to previous treatments, effects of side during treatment. Age of onset, extra-gastrointestinal manifestations and duration of disease are also important factors. The sum of these factors helps to group patients including severe patients requiring inpatient treatment and patients with mild to moderate disease who can be managed as an outpatient. Use of the Truelove and Witts classification in clinical practice has been proven and is now a widely used indicator. In some settings, a erythrocyte sedimentation rate > 30 mm/hr can be replaced by a CRP > 30 mg/l. To assess disease activity, some guidelines for the use of the Mayo scale are developed on factors such as bowel frequency, rectal bleeding, endoscopic imaging, and general assessment in which, if no results are obtained, Endoscopic findings, using an incomplete Mayo score are still clinically relevant. During follow-up, the definition of treatment response, remission as well as treatment resistance is important in optimizing and modifying treatment regimens. The 2015 Toronto Consensus provided definitions for these.Definition of treatment response levels according to the Toronto consensus
| Khái niệm | Định nghĩa |
| Hồi phục hoàn toàn | Tất cả các triệu chứng trên lâm sàng và tổn thương trên nội soi đều hồi phục. |
| Hồi phục tồn thương trên nội soi | Niêm mạc bình thường hoặc mạng lưới mao mạch không rõ, có thể có biến đổi mạn tính (polyp viêm, sẹo) nhưng niêm mạc không dễ chảy máu. |
| Lui bệnh về triệu chứng lâm sàng | Số lần đại tiện bình thường (<3 lần/ngày), phân không có máu. |
| Đáp ứng về triệu chứng lâm sàng | Có sự cải thiện về triệu chứng lâm sàng do chính bệnh nhân và bác sĩ đánh giá, có thể coi là tiêu chí đánh giá đáp ứng điều trị sớm. |
4. Diagnosis of severe bleeding ulcerative colitis
Severe cases require hospitalization for comprehensive care. The patient is considered severe when he has bloody stools 26 times/day and has one of the symptoms of systemic toxicity (pulse > 90 beats/min, temperature > 37.80C, Hb < 105g/l, blood velocity) 30mm/hr or CRP>30mg/l). Patients with comorbidities or over 60 years of age have a higher risk of death. The patient should be excluded from infectious diseases.
5. Treatment of severe bleeding ulcerative colitis
Intravenous steroid therapy is recommended as a first-line regimen with methylprednisolone 60 mg every 24 hours or hydrocortisone 100 mg four times a day. Intermittent bolus or intravenous infusion are equally effective. An alternative steroid treatment option is intravenous cyclosporine at a dose of 4 mg/kg/day. A randomized controlled trial demonstrated the efficacy of intravenous cyclosporine to be equivalent to methylprednisolone in severe disease progression. Therefore, treatment may be considered when patients cannot use steroids such as those with osteoporosis or severe, difficult-to-control diabetes. In addition to steroid treatment, during monitoring and treatment of critically ill patients, the ECCO's recommendations should pay attention to the following points:
Monitor and adjust to prevent water and electrolyte disturbances. Decreased potassium or magnesium will promote the progression of toxic megacolon. Potassium supplementation of at least 60mmol/day is necessary. CMV infection should be ruled out by sigmoidoscopy with biopsy when patients have flares of steroid-resistant disease. Stool culture to rule out c.difficile is also required because in case of positive, oral vancomycin and immunosuppressive agents should be temporarily discontinued. Administration of low molecular weight heparin subcutaneously during severe acute exacerbations helps to prevent the risk of thrombosis. Nutritional support if the patient is undernourished, in which enteral nutrition is preferred due to physiological suitability as well as lower complication rate than parenteral nutrition (9% vs. episode of acute colitis). Discontinue anticholinergics, antidiarrheals, NSAIDs, and opioids that may aggravate dilatation of the colon. Topical agents such as steroids or 5-ASA combinations can be used if tolerated. Use antibiotics only if there is an infection or preoperative prophylaxis. Blood transfusion to maintain Hb levels above 8g/dl and specialist consultation with surgeons to select surgical or conservative treatment options. Vinmec International General Hospital is a prestigious examination address with a team of highly qualified medical professionals, along with modern medical equipment of international standard quality, readers can trust to choose to do the work. destination for examination and treatment for yourself and your family.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference article : De Dombal F.T. (1968), Ulcerative colitis: definition, historical background, aetiology, diagnosis, naturel history and local complications, Postgrad Med, Lichtenstein G.R., btv. (2014), Medical Therapy of Ulcerative Colitis, Springer-Verlag, New York, Crohn B.B. (1962). An historic note on ulcerative colitis. Gastroenterology, 42, 366-367.