This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Inflammatory bowel disease (IBD) is a chronic and idiopathic inflammatory disease of the gastrointestinal tract that shows an episode of remission and recurrence. Ulcerative colitis (UC) and Crohn's disease (CD) are the two main forms of inflammatory bowel disease. The number of IBD patients has increased rapidly in recent years and is increasingly prominent in Korea. However, many physicians still do not fully understand the clinical and endoscopic features of inflammatory bowel disease, so diagnosis is often delayed or inaccurate in many cases.
1. Overview of inflammatory bowel disease and ulcerative colitis
Accurate diagnosis of inflammatory bowel disease is an increasingly important issue. Diagnostic guidelines for inflammatory bowel disease were established by the Inflammatory Bowel Disease Study Group of the Korean Intestinal Diseases Research Association in 2009.
Hospitalized patients with acute severe ulcerative colitis require a group approach multidisciplinary, focusing on early escalation of medical therapy and early surgical consultation. This review provides a practical overview by physicians in the inpatient treatment of severe acute ulcerative colitis.
2. What is severe ulcerative colitis?
Acute severe ulcerative colitis (UC) is a medical emergency requiring hospitalization and a multidisciplinary team approach involving a gastroenterologist and colorectal surgeon. North American UC cohort studies report that 18 to 25% of patients with UC will experience at least one flare-up requiring hospitalization.
Severe UC was defined as six or more bloody stools per day, tachycardia, fever, anemia (hemoglobin < 10g/dL), and high erythrocyte sedimentation rate (ESR > 30).

3. Assess and treat patients on the first day
At initial presentation, the patient should be hemodynamically resuscitated when appropriate.
3.1. Evaluation of stool for infectious pathogens Patients should have a stool sample tested for Clostridium difficile (C. difficile) and cultured for the causative organism. Patients with inflammatory bowel disease (IBD) concurrently infected with C. difficile require longer hospitalization, increased resection requirements, and higher mortality. Stool samples should be obtained first and if clinical suspicion of C. difficile infection is high, prophylactic oral vancomycin can be initiated. Oral vancomycin should be discontinued if C. difficle is negative. Routine antibiotic use in the absence of infectious colitis is not appropriate.
3.2. Laboratory evaluation On admission, the laboratory must include a complete blood count (CBC), basal metabolic panel (BMP), and albumin. C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) should be ordered to assess disease severity. Some patients may have a normal CRP despite severe inflammation on endoscopy.
To prepare for possible biologic therapy, one should be tested for tuberculosis (QuantiFERON-TB Gold and chest X-ray), hepatitis B (hepatitis B surface antigen, hepatitis surface antibody). B and hepatitis B core antibody) and human immunodeficiency virus (HIV antibody). Some of these tests take several days to get results; Therefore, it is best to attract them upon admission.
3.3. Abdominal radiograph Patients should have a simple abdominal radiograph initially upon admission to help identify conditions requiring immediate surgical care such as megacolon, pneumococcal enteritis, and perforation. If the patient's clinical course changes at any time during the hospital stay, it is important to have the abdominal radiograph repeated and compared with the baseline.
3.4. Endoscopic evaluation Pelvicoscopy with biopsy should be performed within the first 48 hours to assess disease severity and biopsy for cytomegalovirus (CMV). Bowel preparation and total colonoscopy are unnecessary in the acute phase and may increase the risk of colonic disease and perforation.
Biopsy for CMV should be done in the center of the ulcer. The gold standard for diagnosis is immunohistochemistry. CMV was considered significant if there were more than five virus individuals per field. The preferred treatment for CMV colitis is IV ganciclovir.
3.5. Diet Patients should be able to eat a normal diet for the duration of their hospital stay. There is no evidence that complete bowel rest or total parenteral nutrition (TPN) improves inflammation or changes disease outcome. If a normal diet is not tolerated, parenteral nutrition is indicated.
3.6. Prophylaxis of DVT Hospitalization and active inflammation increase the risk of deep vein thrombosis (DVT) in UC patients. In a meta-analysis of eight randomized controlled trials, there was no significant increase in bleeding in patients treated with heparin during hospitalization due to an acute flare of UC. Therefore, despite the presence of bloody stools, all hospitalized UC patients should receive DVT prophylaxis.
3.7. Initial medical therapy with IV corticosteroids (40mg/day) should be initiated on admission. Studies have shown that there is no evidence to support an increase in methylprednisolone beyond 60 mg/day and that the benefits do not outweigh the risks when the dose is increased beyond 40 mg/day.
Patients who do not respond to intravenous corticosteroids by day 3 have poor outcome and need to be evaluated for surgery or medical treatment. Nonresponse to steroids was defined as ≥8 stools/day or 3-8 stools/day plus CRP >45 mg/L on days 3. 4
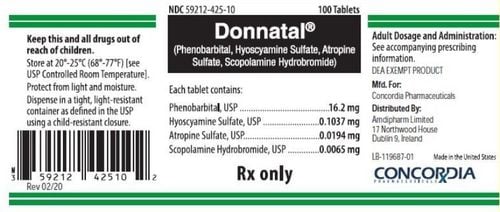
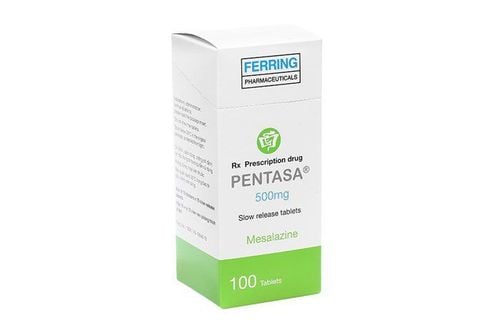
3.8. Drugs to be avoided and/or discontinued on admission Aminosalicylate has been shown to cause paradoxical colitis in 3% of patients and should therefore be discontinued on admission. Nonsteroidal anti-inflammatory drugs (NSAIDs) can cause ulcers, increase the risk of gastrointestinal bleeding, and may worsen flare-ups and should be avoided.
Morphine increases morbidity and mortality in IBD patients. It may also increase a patient's risk of megacolon. It is best to avoid drug use. Antidiarrheal drugs can also alter colonic motility and have no role in the treatment of UC.
4. Evaluation and treatment of patients on day 2
4.1. Clinical and laboratory evaluation Clinical response should be assessed based on trends in stool counts, fecal blood, and CRP.
4.2. Colorectal Surgery Counseling Early colorectal surgery counseling is important. Surgery should be considered as an option for the treatment of patients unresponsive to intravenous corticosteroids. Early discussion of all possible options (medical or surgical) between the patient, the colorectal surgeon, and the gastroenterologist will ensure optimal patient care.

5. Evaluation and treatment of patients on day 3
5.1. Clinical and laboratory evaluation On day 3, response to intravenous corticosteroids helps determine if emergency therapy (medical or surgical) is needed. Patients who are responding to intravenous corticosteroids as defined by less than 8 stools per day with an appropriate decrease in CRP may be switched to oral prednisone (40 mg daily). These patients should be discharged with oral prednisone (40 mg daily) and closely monitored for outpatient gastroenterology (preferably within one week). At follow-up, maintenance therapy (biologic and/or immunomodulatory) should be initiated and prednisone tapered gradually.
Patients who do not respond to intravenous corticosteroids by day 3, as defined by ≥8 stools/day or 3-8 stools/day plus CRP >45 mg/L, should consider alternative medical therapy because of surgery. 4
5.2. Rescue therapy Cyclosporine IV or infliximab is appropriate as salvage therapy for patients who have failed IV corticosteroids and should be administered on days 3-5. The choice of drug depends on the expertise and existing conditions of the center. Response should be assessed within 5-7 days of receiving rescue medical therapy. If there is no clinical response on day 7, surgery is indicated.
Patients who respond to IV cyclosporin should be switched to oral thiopurines for maintenance therapy. Combination therapy with biologics may be required. Patients who respond to an infliximab infusion should complete the initiation doses at weeks 2 and 6, followed by maintenance therapy every 8 weeks. Combination therapy with an immunomodulator should be considered.
Low albumin levels and high CRP are associated with lower serum infliximab concentrations due to rapid clearance. Studies have also found that infliximab is lost in the stool during severe inflammation resulting in lower serum concentrations of infliximab. Therefore, higher and more frequent doses of infliximab may be required in patients with acute severe UC with elevated CRP levels and hypoalbuminemia. A recent retrospective study showed that accelerated dosing of infliximab (5 mg/kg infliximab, 3 doses over a median of 24 days) was associated with a lower incidence of hysterectomy compared with the standard infliximab induction dose ( infliximab 5mg/kg at weeks 0, 2 and 6).

5.3. Surgical management Indications for surgery include toxic megacolon, colonic perforation, massive bleeding, failure to respond to intravenous corticosteroids on day 3, and failure to respond to medical treatment with cyclosporin or infliximab. The surgery of choice was total colectomy with percutaneous ileostomy and the creation of a Hartmann pouch in the pelvis. Restoration of bowel circulation can be done three to six months after the initial colectomy. CONCLUSION All patients with acute flares of severe UC requiring hospitalization should receive intravenous corticosteroids on admission. C. difficile infection is common and should be treated with oral vancomycin. An early multidisciplinary team approach is critical to ensuring optimal patient outcomes. Early emergency medical therapy or surgery is indicated if the patient does not respond to intravenous corticosteroids by day 3. Other biologics have not been studied as thoroughly as emergency medical therapies. Future research should be directed towards characterizing the use of biosimilars and other biosimilars in the setting of acute flares of severe ulcerative colitis requiring hospitalization.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit examination and treatment at the Hospital.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Dinesen LC, Walsh AJ, Protic MN, et al. The pattern and outcome of acute severe colitis. J Crohn's Colitis. 2010;4(4):431-437. Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1963;4:299-315. Turner D, Walsh CM, Steinhart AH, Griffiths AM. Response to corticosteroids in severe ulcerative colitis: A systematic review of the literature and a meta-regression. Clin Gastroenterol Hepatol. 2007;5(1):103-110. Travis SP, Farrant JM, Ricketts C, et al. Predicting outcome in severe ulcerative colitis. Gut. 1996;38(6):905-910. Stephanie O. Eschette et al., A Practical Approach to Managing Inpatient Acute Severe Ulcerative Colitis, Practical gastroenterology • october 2017