This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Cao Thi Thanh - Pediatrician - Department of Pediatrics - Neonatology - Vinmec Hai Phong International General Hospital.1. What is necrotizing enterocolitis?
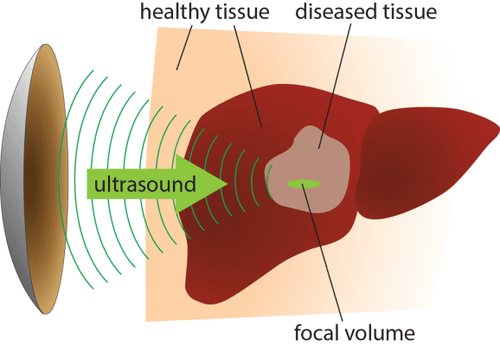
Necrotizing enterocolitis is a condition in which the intestines become infected and may begin to become necrotic. This is an acute intestinal disease, common among children's digestive diseases, especially premature babies (accounting for 70-80% of children with low gestational age). Babies born at full term can also get this disease, but less often.If the disease is not detected and treated promptly, the intestinal wall will necrosis, causing intestinal perforation, gastrointestinal effusion into the abdominal cavity, leading to intestinal obstruction, peritonitis. These complications can be fatal and require immediate surgery.
The cause of neonatal necrotizing enterocolitis is unknown. However, there are many factors involved in the disease including: Prematurity (premature babies' intestines are not as mature as full-term babies), infections, damage to blood vessels, reduced blood flow to the intestines, asphyxia at birth. , postpartum respiratory failure, congenital heart disease, metabolic abnormalities, abnormal fetal development, hypothermia, infant formula feeding,...
Trắc nghiệm: Thế nào là trẻ sơ sinh non tháng?
Trẻ sơ sinh non tháng rất cần được chăm và điều trị thật tốt để giúp giảm nguy cơ gặp phải các di chứng về tinh thần, vận động và sự phát triển sau này. Cùng theo dõi bài trắc nghiệm dưới đây để có thể nhận biết trẻ sơ sinh non tháng và có thêm kiến thức chăm sóc, nuôi dưỡng tốt nhất cho trẻ.The following content is prepared under supervision of Thạc sĩ, Bác sĩ y khoa, Ma Văn Thấm , Nhi , Phòng khám Đa khoa Quốc tế Vinmec Dương Đông(Phú Quốc)
2. Diagnosis of necrotizing enterocolitis in preterm neonates
2.1 Diagnosis based on clinical symptoms Early stage: Lethargy, lethargy, unstable temperature, abdominal pain above or around the navel, slow digestion of gastric juice, fluid retention about 20%. The child has short episodes of apnea, the heart rate may be slow, and the blood sugar is low; The next stage: Children vomit yellow fluid, pale skin, severe abdominal pain, diarrhea, sometimes whole or microscopic blood in the stool. Accompanied by symptoms of abdominal distension, rectal examination is sometimes bloody. Late stage: The gastric juice is dark brown, with shock, severe abdominal pain, distended abdomen, erythematous wall, peritoneal tenderness, peritonitis.
3. Treatment of necrotizing enterocolitis in preterm infants
3.1 Medical treatment Medical measures should be taken as soon as there are signs that the patient has necrotizing enterocolitis, without waiting until the diagnosis is certain to avoid missing the opportunity to treat the disease early. Methods include:Oral fasting: inserting a nasogastric tube to drain gastric juice. Resume oral feeding only when the clinical improvement is good (no bleeding, no abdominal distention) or at least 5 days after abdominal X-ray shows that the disease is under control (no longer intestinal gas. ). If an umbilical vein catheter is in place, the catheter should be removed. Combined with electrolyte replacement, anti-shock, treatment of DIC. When hemodynamically stable, switch to total parenteral nutrition for 1 - 2 weeks; Initial antibiotics: Use Ampicillin + Cefotaxime/Gentamicin + Metronidazol. If there is no response, the antibiotic should be changed according to the antibiogram. If antibiogram is not available, use pefloxacin in combination with metronidazole. The duration of antibiotic use for pediatric patients with necrotizing enterocolitis is 10-14 days; Close follow-up: Clinical signs of bowel obstruction, abdominal circumference, abdominal X-ray every 8-12 hours in unstable disease stage to promptly detect surgical complications and have timely treatment plans time, efficiency.

4. Measures to prevent necrotizing enterocolitis in premature infants
Pregnant women should have regular antenatal check-ups according to the doctor's appointment. It is necessary to detect pregnant women at high risk of comorbidities during pregnancy or underlying medical conditions in the mother for effective prevention; Having a specific strategy on treatment and care for pregnant women to help the fetus in the womb have good health and develop in accordance with each stage of pregnancy; Avoid premature birth. It is necessary to understand the cases of birth early compared to the due date to have a good treatment, to help the fetus develop well; Avoid other risks during and after birth such as: asphyxia, prolonged respiratory failure, polycythemia in premature infants; Care should be taken when feeding preterm infants by enteral feeding because feeding them in large quantities, rapidly increasing the quantity with unreasonable time is a risk of causing necrotizing enterocolitis. Children should eat slowly with each meal in small amounts. Good regulation of the time and amount of milk in the meal can prevent necrotizing enterocolitis. The amount of milk should be gradually increased to no more than 20ml/kg/day. At the same time, it is necessary to monitor and evaluate the child's milk tolerance status; Babies need to be breastfed right in the first hours after birth because breast milk contains many protective factors such as IgA, IgG, IgM,... that help reduce the risk of necrotizing enterocolitis in premature babies. Mothers should exclusively breastfeed their babies day and night. In order to have an abundant milk supply, pregnant women need to eat nutritious food, focus on protein, and get enough rest and sleep.
Pediatrics department at Vinmec International General Hospital is the address for receiving and examining diseases that infants and young children are susceptible to: viral fever, bacterial fever, otitis media, pneumonia in children, .... With modern equipment, sterile space, minimizing the impact as well as the risk of disease spread. Along with that is the dedication from the doctors with professional experience with pediatric patients, making the examination no longer a concern of the parents.
Doctor Thanh has worked for 25 years in the treatment of neonatal pediatric diseases, of which 23 years worked at the neonatal department of Hai Phong Obstetrics and Gynecology Hospital (with experience in neonatal resuscitation in the operating room/room). giving birth + taking care of late premature babies (34 weeks - 37 weeks), 02 years working at Hai Phong Children's Hospital Requesting Clinic.Dr. Thanh is currently working in Pediatrics - Neonatology Department of International General Hospital Vinmec Hai Phong
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.