This is an automatically translated article.
The article was professionally consulted by MSc Vu Thi Tuyet Mai - Cardiologist, Vinmec Central Park International General Hospital.Acute heart failure is a condition in which the symptoms of heart failure syndrome occur suddenly. The patient needs immediate emergency care and intensive resuscitation, otherwise it will be life-threatening.
1. What is acute heart failure?
Acute heart failure is a condition in which the manifestations of heart failure syndrome occur suddenly, requiring emergency intervention as quickly as possible. Symptoms include pulmonary congestion and possibly decreased systemic cardiac output. There are now significant advances in the diagnosis and treatment of acute heart failure.
Acute heart failure can be acute pulmonary edema or cardiogenic shock. New-onset acute heart failure accounts for 20%, the remaining 80% is decompensated acute heart failure on the background of chronic heart failure. Therefore, it is necessary to identify the type of heart failure, the predisposing factors and the causes leading to acute heart failure in order to have a reasonable treatment approach.
2. Causes of acute heart failure

3. Symptoms
Symptoms related to volume overload:
Shortness of breath (on exertion, paroxysmal nocturnal, lying, or at rest); cough, wheeze. Discomfort in the legs and feet: edema, numbness, cold Abdominal discomfort: abdominal fullness, loss of appetite On examination, you will find: rales in the lungs, pleural effusion, peripheral edema (legs, lower regions), abdominal distention or increased abdominal circumference, right upper quadrant pain or tenderness, hepatomegaly or splenomegaly, yellow sclera, weight gain, jugular venous distension, jugular venous return (+), increased T3 sound, strong T2 sound . Symptoms related to tissue hypoperfusion:
Fatigue Changes in consciousness, daytime somnolence, confusion, loss of concentration, dizziness, near fainting or fainting Cold hands and feet, pale, low blood pressure Examination reveals: narrow pulse pressure or low differential pressure, shock.

4. Treatment of acute heart failure
Assess the patient for respiratory failure or cardiogenic shock, if necessary, resuscitate and transfer the patient to the ICU.
In milder cases of acute heart failure, assess the patient's airway, ventilate and oxygenate the patient, place an intravenous line and administer medication, assess the patient's vital signs, monitor the patient's urine patient.
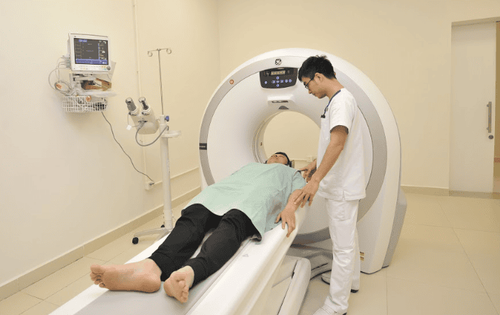
4.1. Acute pulmonary edema Assessment of patients with acute pulmonary edema through the following factors:
History, physical symptoms and physical examination Tests for diagnosis and risk assessment: 12-lead electrocardiogram, X-ray - Chest radiograph, transthoracic echocardiography, blood count, blood urea, blood creatinine, electrolytes, cardiac enzymes, arterial blood gases. In-depth invasive tests: cardiac catheterization, transesophageal echocardiography, systemic artery or pulmonary artery catheterization are necessary in severe, complicated clinical situations. Treatment measures include:
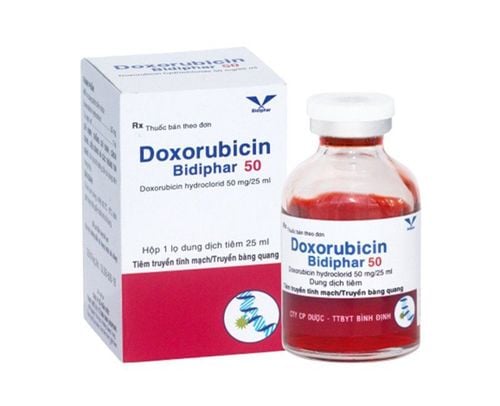
Oxygen. Place intravenous line and use injectable drugs such as: diuretic Furosemide, Nitroglycerin, Morphine Sulfate. Infusion of vasopressors such as Dobutamine, Dopamine when hemodynamic instability. Intubation and mechanical ventilation if severe hypoxemia is unresponsive to treatment and respiratory acidosis is present. Circulatory support by mechanical means. Ultrafiltration of blood. Treat the cause of acute pulmonary edema. After the patient is out of the acute pulmonary edema, seek to determine the cause for long-term treatment. 4.2. Cardiogenic shock The cardiac damage that leads to cardiogenic shock may be in the myocardium, heart valves, chambers, or due to arrhythmias. In patients with acute myocardial infarction, 80% of cardiogenic shock is due to myocardial damage, only 20% due to mechanical factors such as acute mitral regurgitation, perforation of the interventricular septum.
Evaluation of patients with cardiogenic shock:
History, physical examination. Hemodynamic assessment: systolic blood pressure <90 mmHg lasting for more than 30 minutes, cardiac output index <1.8 l/min/m2 and left ventricular filling pressure > 20 mmHg. Laboratory investigations to do: 12-lead electrocardiogram (including right thoracic lead), chest X-ray, echocardiogram, central venous pressure measurement, Swan-Ganz tube insertion, formula blood, blood urea and creatinine, liver enzymes, heart enzymes, electrolytes, arterial blood gases, blood lactate, coagulation tests. Treatment measures include:
Oxygen inhalation. Intubate and help with mechanical ventilation if needed. Intravenous vasopressors: Dopamine, Dobutamine, Milrinone, Noradrenaline Aortic counterpulsation ballooning Mechanical circulatory support, ventricular assist device, extracorporeal membrane oxygenation system ECMO. Coronary revascularization (bypass, dilation and stenting) if cardiogenic shock due to myocardial infarction.
5. Follow-up treatment

Continue treatment to improve the patient's hemodynamics, volume, and clinical symptoms of acute heart failure. The patient was then treated for chronic heart failure. Patients need to reduce the time of intensive care, adjust medication and monitor hemodynamics, weight, volume of fluid in and out every day for the patient.
Acute heart failure is a life-threatening medical condition that requires prompt and timely access to diagnosis and management. In addition, the post-discharge follow-up is associated with the disease management program and the follow-up plan of hospitals and doctors, which play an important role in reducing symptoms, improving quality of life, reducing re-hospitalization and reduced risk of death for the patient.
Currently, the percentage of patients with heart failure is increasing, progressing faster. Therefore, finding a specialist clinic or hospital is essential. Cardiovascular Center - Vinmec Times City International Hospital has built a Heart Failure Intensive Care Clinic which has been organized and put into operation since March 2019. This is one of the few specialized heart failure clinics built the earliest in Vietnam with reference to the US and Singapore models, bringing hope of effective treatment for patients with heart failure in order to serve for the needs of examination, consultation and treatment to bring health to patients.
Patients are managed according to a unified medical record form, which is convenient for searching and storing on the principle of confidentiality. The hospital is building software on smartphones through which to have close and regular interaction between patients and medical staff such as: appointment reminders, reminders and instructions for taking medicines, how to use them. management of emerging situations, health education.
Assess the degree of heart failure, make a specific, optimal and appropriate treatment plan for each patient, on the basis of applying updated guidelines from major Cardiology organizations in the world such as the American Heart Association. European Heart Association, American College of Cardiology and Cardiology. For patients with late-stage heart failure, the heart failure specialist clinic will hold consultations to offer enhanced treatment measures: resynchronization, ventricular assist devices, heart transplantation.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.