This is an automatically translated article.
Article by Doctor, Doctor Hoang Minh Duc - Vinmec Stem Cell Research Institute and Gene Technology
The appearance of a storm of cytokines in patients infected with Covid-19 is one of the typical examples of acute pneumonia that provokes a storm of cytokines that release these active substances into the circulatory system and make the patient's condition worse. more critical.
1. What is Cytokine storm?
The term “cytokine storm” or “cytokine storm” is a scientific term that was first used in a 1993 scientific paper describing the process of an intense immune system response in a study of Graft-versus-host disease.
However, by the beginning of the 21st century, this phrase was used frequently in research related to infectious diseases, especially infectious diseases related to viruses such as cytomegalovirus, Epstein-Barr virus, group A streptococus, infuenza virus, variola virus, and pneumonia virus (SARS-CoV). After the H5N1 bird flu epidemic in 2005, this phrase was widely used by scientists in in-depth research.
Theoretically, a cytokine storm is defined as a sudden and uncontrolled increase in a large amount of cytokines secreted by cells of the immune system due to stimulation by various agents, especially is in infection and the body's response to viral attack. To better understand the mechanism of cytokine storm, we must first understand the definition of cytokines.
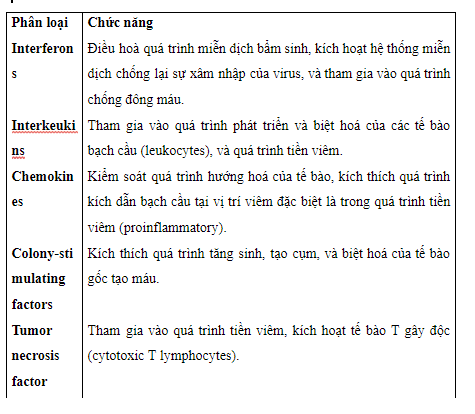
Cytokines are a diverse population of protein active substances secreted from cells for the purpose of conducting intracellular signals and directly participating in the communication process between cells in the body (cell-cell). communication). The function of cytokines is based on 03 main mechanisms: Autocrine (self-activating mechanism of cells - cytokines are secreted from the mother cell and activate the cell itself), paracrine (the mechanism of activation of cells). surrounding – cytokines are secreted from a cell and act on the cells around it), and endocrine (endocrine activation mechanism – cytokines are secreted from one or more cells and act on the cells) Targets are located at different locations on the body).
The important functions of cytokines are their ability to participate in the control of cell proliferation and differentiation in the body and the ability to trigger immune responses. The functions of cytokines are classified according to their purpose of action as shown in Table 1.
The storm of cytokines in the immune response usually begins with inflammatory reactions at the site of injury and then rapidly spreads to the whole body through the circulatory system. The acute immune response (Acute inflammation) is composed of five steps: Rubor (redness), tumor (swelling), calor (raising temperature at the site of inflammation), dolor (pain), and "functio laesa" (loss of pain). functioning function).
In acute lung injury, a storm of cytokines begins to land on the inflammatory site in the alveoli, activates the immune process, and attracts almost all cells in the immune system at the site of inflammation. secrete cytokines to fight inflammatory factors such as viruses. Because the lungs are the gas exchange organs of the whole body, so with the intricate system of blood vessels and capillaries and a complex lymphatic network, the release of active cytokines into the blood is easy and quick. This leads to dilution of cytokines in the alveoli carried by the blood to other sites of the body, activating more white blood cells to secrete more cytokines and ultimately triggering a systemic immune response. system if the inflammatory agent cannot be controlled.
Therefore, for cases of acute viral pneumonia, acute respiratory distress syndrome (ADRS) is the result of an uncontrolled inflammatory process in the lungs caused by a viral attack (such as SARS- CoV or influenza) leads to the activation of a storm of cytokines. The appearance of a storm of cytokines in patients infected with Covid-19 is one of the typical examples of acute pneumonia that provokes a storm of cytokines that release these active substances into the circulatory system and make the patient's condition at risk. more dramatic.
2. Cytokine storm in COVID-19
When alveolar cells are attacked by the Covid-19 virus, they will activate macrophages that reside in the lungs. These macrophages secrete IL-6, IL-10, and TNFα which increase alveolar concentrations of these active substances leading to the attraction of CD4+ and CD8+ T cells from blood vessels entering the alveoli from which initiates the process of hemophagocytosis (hemophagocytic lymphophistiocytosis).
In most severe cases when attacked by Covid-19, cytokines that tend to increase include IL-2, IL-7, granulocyte-colony factor, INF-γ inducible protein 10, monocyte chemoattractant protein 1, macrophage inflammatory protein 1-α, and tumor necrosis factor-α. In addition, when macrophages and T cells are activated, the secretion of other cytokines such as IL-06, IL-2R, IL-10 and TNFα is increased. This loop is repeated because the viral load on the alveoli is not reduced, leading to the activation of a storm of cytokines in the alveoli and a decrease in the number of CD4+ and CD8+ T cells. In fact, these two types of cells in the body of patients with severe Covid-19 infection tend to decrease sharply.
3. Mechanism of MSCs in Cyclone Regulatory Cytokines
Mechanistically, based on preclinical studies and basic scientific studies, several mechanisms are proposed when alveolar cells are attacked by pathogens such as bacteria and viruses .
3.1 Anti-inflammatory mechanism Anti-inflammatory mechanism, also known as “immunoregulatory mechanism” is one of the mechanisms that create the unique characteristics of mesenchymal stem cells when applied in clinical practice. . In a study on a mouse model of pneumonia, the active substance IL-01ra secreted from MSCs was able to inhibit the activation of helper T cells and at the same time inactivate its production. TNFα of intrapulmonary macrophages. In addition, MSCs also secreted TSG-6, which participates in the reduction of cytokines secreted by macrophages in a model of pneumonia. MSCs also secrete IGF-1, which participates in immune regulation by regulating macrophage proliferation.
3.2 Regulation of permeability of alveolar endothelial cells Alveolar endothelium injury is one of the features of acute pneumonia (ADRS) leading to pulmonary effusion and the release of cytokines into the blood vessels blood. Stem cell infusion into animal models of pneumonia showed the ability to protect alveolar endothelial cells during apoptosis or necrosis preserving integrity. of the alveoli.
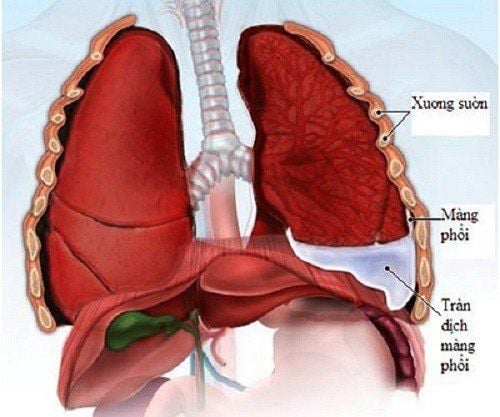
3.3 Regulation of permeability of alveolar epithelial cells (epithelial cells) Alveolar epithelial lining is composed of 2 types of epithelial cells type 1 and type 2. The process of mucosal epithelial damage. is one of the causes of ADRS which directly affects alveolar integrity and disrupts alveolar and vascular barriers.
MSCs cells when co-cultured with damaged alveolar cells have the effect of reversing the absorption of immunoactive substances such as IL-01, TNFα and interferon-gamma, helping the alveolar cells. are not attacked by immune cells. In addition, MSCs also secrete Angiopoietin-1 (AnG-1), the active substance involved in stabilizing endothelial cells and helping to keep alveolar epithelial cells from breaking down.
4. Increases the process of eliminating fluid inside the lungs
The process of eliminating the fluid inside the alveoli is one of the important steps to restore the alveoli after injury. These fluids are usually eliminated through a complex capillary system in the alveoli. Many studies have shown that MSCs secrete FGF-7 which activates the secretion of fluid inside the alveoli.
4.1 Anti-inflammatory In addition to immunoregulatory processes, MSCs are known for their ability to fight inflammation from extracellular bacterial infections. The anti-inflammatory potential of MSCs is partly due to the activation of immune cells in the alveoli such as monocytes, neutrophils and macrophages) to attack and eliminate inflammatory factors. In addition, the ability to secrete antimicrobial peptide lipocalin-2 also showed the ability to prevent bacterial attack.
4.2 Anti-Apoptotic Apoptotic processes of immune cells and alveolar cells are very common in ARDS conditions. The interaction between these MSCs and these cells as well as through the secretion of the active substance FGF-7 suggests the ability to support the regulation of cell apoptosis and increase the cell's ability to recover. injury.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.