This is an automatically translated article.
Article by Master, Doctor Le Thai Bao - Department of Intensive Care - Vinmec Times City International Hospital
Currently, mechanically ventilated patients, weaned from mechanical ventilation by CPAP test or T-tube (T-tube) are often used in clinical practice to avoid hospital-acquired infections, ventilator-associated lung damage, extremities, etc. Expensive treatment costs make it difficult to leave the device and the patient is at risk of death.
1. CPAP . self-breathing test technique
Prolonged mechanical ventilation will lead to nosocomial infections, ventilator-associated lung damage, expensive treatment costs that make it difficult to remove the machine and the patient is at risk of death. Therefore, every time a patient is on a ventilator, the operator needs to quickly assess the patient's weaning from the ventilator to consider quitting the ventilator as soon as possible.
Currently, in mechanically ventilated patients, weaning from mechanical ventilation by CPAP test or T-tube (T-tube) are commonly used in clinical practice.
2. Designation

Patients breathing PSV respond well to PS ≤ 5cmH2O Patients breathing SIMV respond well to a rate of 6 beats/min, PS 5 cmH2O Patients on mechanical ventilation, the cause of need for mechanical ventilation has been resolved, for example: After surgery, convulsions... The patient meets the criteria for weaning off mechanical ventilation
3. Contraindications
Patient stops breathing, stops heart Patient is unable to breathe on his own (such as severe neuromuscular disease...) Not meeting the criteria for weaning off mechanical ventilation
4. CPAP . self-breathing test technique
4.1. Preparation Person: 01 Doctor and 01 nurse specializing in Emergency Resuscitation or trained in mechanical ventilation.
Facilities:
Consumables:
Ventilator oxygen (24-hour running day) Bacterial filter on ventilator line: 01 piece Serum line: 01 piece Sterile gloves: 03 pairs Clean gloves: 05 pairs N2 minor surgical gauze: 05 bags Surgical mask: 03 pcs Surgical cap: 03 pcs MDI adapter: 01 pcs Ventilator wire set: 01 set of Compressed air (24-hour running day) Thermohumidifier: 01 pcs Dust filter ventilator: 01 pcs Savondoux soap for hand washing First aid kit:
01 pleural opener for air drainage Other expenses:
Consumption of electricity, water Fees for steaming, washing tools Handling medical waste and garbage Living

Patient:
Explain to patient (if patient is conscious) and family/legal representative of patient about the need and risks of mechanical ventilation. The patient/patient's representative signs a commitment to perform the technique. Patient position: The patient lies with the head elevated 30 degrees (if there is no drop in blood pressure), the head is flat if the blood pressure is low Ventilation at the hospital bed Medical record:
Explain the technique to the patient and family the patient and sign the agreement to agree to the technique, the record of the procedure monitoring.
4.2 Procedures Checking the record: Rechecking indications, contraindications and consent to participate in the technique Re-checking the patient: Vital functions, see if the procedure can be carried out . 4.3 Perform the technique Fully record the parameters of the ventilator mode being performed before switching to the weaning mode
Criteria for mechanical weaning:
Solve the cause of the need for mechanical ventilation Improve blood oxygenation improvement: PEEP ≤ 5cmH2O, PaO2 > 60 mmHg, with stable FiO2 < 0.5 BP: do not use or use small doses of vasopressors, heart support. Heart rate <140 cycles/min Temperature < 38 degrees C pH and PaCO2 are consistent with the patient's underlying respiratory disease When the patient meets the criteria for weaning off mechanical ventilation. Weaning from mechanical ventilation Weaning from mechanical ventilation:
FiO2 set equal to patient's previous respiratory FiO2 Set CPAP 5 (PS =0 and PEEP=5cmH2O) Assess and adjust ventilator
Rapid shallow breathing index (RSBI) < 100 cycles/min/liter Blood oxygenation: SaO2 ≥ 90%, PaO2 ≥ 60mmHg, pH ≥ 7.32, PaCO2 increase less than 10mmHg compared to before weaning Respiratory rate ≤ 30 cycles/min or change below 50% compared to before. Heart rate < 140 beats/min, or change < 20%, BP Consciousness unchanged, no stimulation. No exertion (use of accessory muscles of respiration, paradoxical breathing)

After 1 hour, if the patient responds to breathing with the CPAP test, remove the device. If the patient coughs, coughs, and is awake, the endotracheal tube should be extubated.
After 1 hour, if patient does not respond to CPAP breathing, return to previous ventilator mode and continue daily CPAP test.
If the patient fails to wean: Need further evaluation:
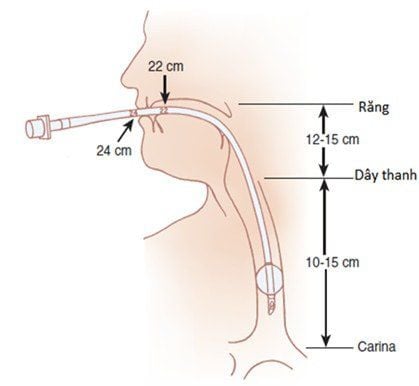
Intubation tube: Check if the endotracheal tube is small?, Is the endotracheal tube blocked?
Blood gas
Avoid metabolic alkalosis in patients with increased PaCO2, keep PaCO2 above baseline value Nutrition:
Support enough energy Avoid electrolyte disturbances Avoid excess energy Sputum:
Clear phlegm Avoid severe dehydration Neuromuscular problems:
Avoid the use of drugs that weaken the muscles (muscle relaxants, aminoglycosides, clindamycin) in patients with muscle weakness Avoid using corticosteroids if not necessary. Airway obstruction:
Exclude airway foreign body Use bronchodilator if necessary Patient awareness: Avoid overdose of sedation
Weaning off mechanical ventilation in the morning
4.4 Post-technological monitoring Machine operation breathing, airway pressures, alarms. Anti-machine status: See if the patient cooperates with the ventilator. If the patient does not cooperate, explain, encourage, and instruct the patient to cooperate with the ventilator. In case of failure, the patient's blood oxygenation does not improve, the patient breathes rapidly > 30 times/min. Switch breathing to control mode.
Pulse, blood pressure, ECG (on monitor), SpO2: Regular. Consciousness of the patient compared to before weaning off the ventilator. Blood gas test: periodically (12-24 hours/time) depending on the patient's condition, emergency treatment when there are abnormal developments. Measure NIF, Vt daily Lung X-ray: Take 1-2 days/time, take emergency scan when there are abnormal developments.
5. Complications and treatment

Consciousness: it is necessary to monitor consciousness to see if the patient is awake (coma: causes of respiratory acidosis, worsening respiratory failure...), if the patient is comatose, check the blood gas again for acidosis respiratory failure and switch back to pre-weaning mode. Breathing rate: If the breathing rate is > 30 times/minute, (with the exception of causes such as sputum obstruction, bronchospasm...) switch to breathing mode before weaning off mechanical ventilation. Low blood pressure: Treat when there is hypotension: give fluids, use vasopressors if necessary. Trauma (pneumothorax): Management: Place emergency pleural drainage. Ventilator-associated infections: Strict adherence to hospital aseptic principles is required for prevention. Start antibiotic treatment early and follow the principle of de-escalation when infection occurs. Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. and hospital treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE
Artificial ventilation (ventilator): What you need to know 2 commonly used methods of artificial ventilation Complications and care for ventilator patients