This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Starting in December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread worldwide as the source of a pandemic. Although the respiratory system is the main apparatus involved in infection, several other organs may be affected in connection with coronavirus disease 2019 (COVID-19).
Human tissues expressing angiotensin-converting enzyme 2 (ACE2) can all be targets of viral damage. In fact, myocarditis, encephalitis-meningitis, acute kidney injury, and other complications have been described in association with SARS-CoV-2 infection. The liver has a central role in the body's homeostasis, contributing to detoxification, catabolism, and the synthesis of important factors such as plasma proteins. ACE2 is significantly expressed only by cholangiocytes in the liver, however transaminases are elevated in more than a third of COVID-19 patients, on admission.
1. Covid-19 and non-cirrhotic chronic liver disease
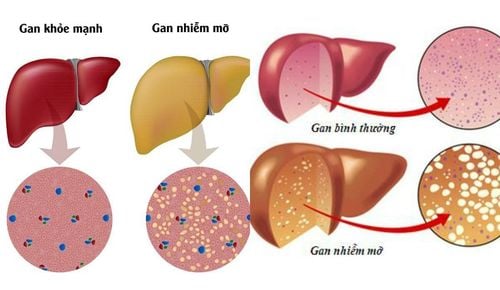
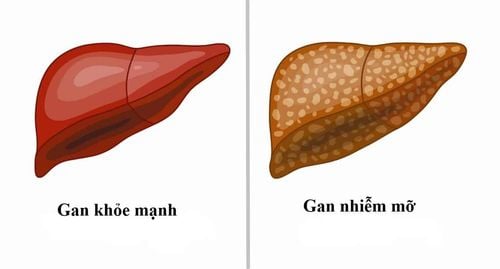
As noted in the previous paragraph, changes in liver function tests during the use of COVID-19 may be the result of different causal events that may act concurrently. When injury occurs in subjects with impaired hepatic reserve, the clinical picture may be more difficult to resolve. Of more interest is the large US study, which included more than 60 million electronic medical records, which also demonstrated that subjects affected by chronic liver diseases (CLD) were more exposed to the acquisition of COVID-19. In this western study, the prevalence of chronic liver disease in COVID-19 patients accounted for 5% of cases, while data from China showed underlying chronic liver disease in 2 to 11% of cases. Several conditions can define chronic liver disease in humans, including those of a metabolic, toxic, viral, or autoimmune nature. Non-alcoholic (or metabolic-related) fatty liver disease (NAFLD), a liver condition that ranges from simple steatosis to nonalcoholic steatohepatitis and is associated with metabolic syndrome, type II diabetes and obesity, which has an estimated prevalence of 25% worldwide. Because of its large burden, the role of NAFLD in determining the extent of liver damage in COVID-19 patients has generated much interest.
Bệnh nhân gan mãn tính khi tiếp xúc với COVID-19 sẽ gây ảnh hưởng
2. What do the studies say?
In China, 70 out of 324 COVID-19 patients (21.6%) were diagnosed with fatty liver during diagnosis by computed tomography. The severity of the clinical picture of COVID-19 is also increased in people with NAFLD. Furthermore, in a retrospective study of 76 COVID-19 patients, the presence of NAFLD was associated with progression of lung failure, with an odds ratio of 6.4. In another study, NAFLD was again associated with a fourfold increased risk of severe COVID-19 exacerbations. The picture linking NAFLD to a severe outcome of this viral infection was then challenged by a study from Qatar. This study, which included 320 NAFLD patients, showed that this metabolic status was only associated with worse outcomes (increased length of ICU stay and requirement for mechanical ventilation) when univariate analysis was used. On the other hand, the main predictor for mortality or worst outcome in multivariate analysis were age >50 and diabetes, respectively. On the basis of the above studies, it is clear why the possible link between NAFLD and severity of COVID-19 remains controversial. The heterogeneity between studies, regarding retrospective enrollment and patient classification, does not contribute to a clear picture. A further analysis may shed light on this issue, linking the degree of liver fibrosis in NAFLD, but not NAFLD, with worse COVID-19 outcomes. In view of this, it seems likely that the degree of liver injury may have a more relevant role than the metabolic disturbance observed in these patients.3. Alcohol abuse disorder often increases the risk of severe progression of SARS-CoV-2 infection in patients with alcoholic liver disease
Alcoholic liver disease (ALD) is an important cause of liver morbidity and mortality worldwide. Despite the fact that clinical data are not available on COVID-19 ALD patients, concern persists about the increased frailty of these subjects during the pandemic. On the other hand, psychological stress and social distancing appear to have increased individuals' alcohol consumption in general. Alcohol abuse disorders often facilitate comorbidities such as viral infections, diabetes, or kidney failure, all factors that can contribute to an increased risk of severe progression with SARS-CoV-2 infection. Furthermore, increased alcohol consumption is considered a risk factor for developing respiratory infections that may complicate the onset of ARDS, one of the key features of severe COVID-19. In addition, during the post-COVID-19 recovery period, prior alcohol abuse is considered a predisposing factor to the development of pulmonary fibrosis. However, there are currently no evidence-based indications for the management of patients with COVID-19 ALD and further studies are needed to improve our understanding of this issue. Currently, expert opinion suggests that, in general, steroid use should be avoided in alcoholic hepatitis while concomitant uncontrolled infections are ongoing, because of the effect of lowering immune defenses. patient translation. On the other hand, in clinical practice, the use of these drugs could be beneficial in the treatment of COVID-19 despite ALD, challenging our pre-SARS-CoV-2 beliefs.
Khi đang trong giai đoạn phục hồi sau COVID-19 nếu lạm dụng rượu sẽ dẫn đến sự phát triển của xơ phổi
4. Challenges associated with the management of autoimmune hepatitis patients with immunosuppressive therapy
Another important challenge concerns the management of patients with autoimmune hepatitis with immunosuppressive therapy. The lack of data from the scientific evidence has encouraged an empiric approach based on dose reduction of immunomodulatory therapy to block the most harmful effects of COVID-19. However, preliminary data from the city of Bergamo, in Italy, do not support this view as no increased risk has been observed in immunosuppressed patients during the SARS-CoV-2 outbreak. On the other hand, it should be considered that it is possible that recurrent autoimmune hepatitis, after tapering immunosuppressive therapy, may require high-dose corticosteroids, significantly increasing the risk of infectious complications in these patients. this multiplier. Therefore, current guidelines do not recommend reducing immunomodulatory therapy in the absence of SARS-CoV-2 infection; In case of excessive infection, the dose can be adjusted to increase the white blood cell count.
5. Covid-19 and other chronic liver disease
Very little data are available on other forms of chronic liver disease. Regarding HBV, in a Chinese series of 105 hepatitis B surface antigen-positive patients hospitalized for COVID-19 (1.9% had cirrhosis, 12.4% on treatment with HBV). antiviral drugs), 14 had significant liver damage. In these subjects, liver injury was associated with an episode of severe infection in nearly 80% of cases. Because of its ability to prevent or reduce COVID-19 should be recognized with the use of antiviral drugs used for hepatitis B virus (HBV) or hepatitis C virus (HCV), one study The Spanish study focused on subjects with chronic viral hepatitis following their specific antiviral regimen, with 1 of 341 HCV patients and 8 of 1764 HBV patients developing COVID -19. Although the majority of them (nearly 80%) were hospitalized, none resulted in death in this group. Finally, it is emphasized that extensive use of intravenous steroid therapy to reduce inflammation can lead to significant HBV reactivation. Routine testing for this virus would be wise in critically ill patients with COVID-19 for prompt prophylactic treatment There are currently no data on the impact of COVID-19 in patients with chronic liver disease. cholestasis, such as primary cholangitis or primary sclerosing cholangitis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.