This is an automatically translated article.
Congenital malformations of the lungs, trachea and bronchi can affect the quality of life or even kill the patient.
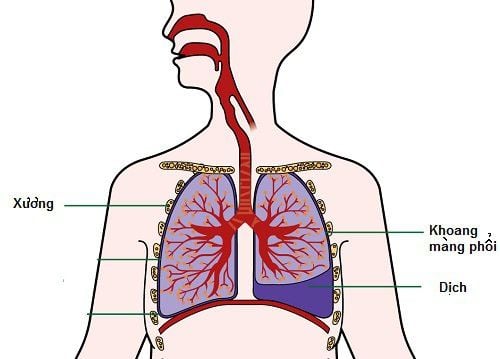
1. Congenital lung diseases
Some common birth defects of the lungs are:
1.1 Deficiency of both lungs In this form of malformation, at birth, the child has only a truncated trachea, completely without bronchi and lungs. Deficiency of both lungs is not clinically significant because babies born with both lungs are not viable.
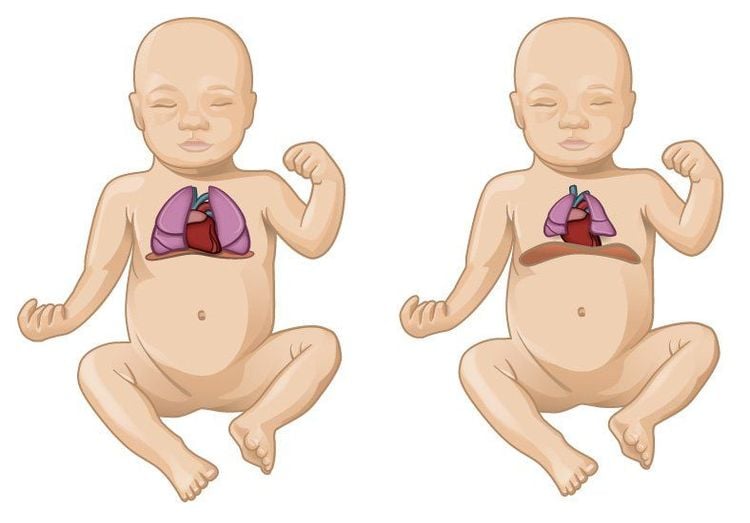
1.2 Deficiency of one lung Deficiency of one lung is often associated with other congenital malformations such as esophageal stricture, diaphragmatic hernia, botanic tube, congenital heart defects,... Children with a missing lung, combined with other birth defects, often die relatively early. About 50% of children with a missing lung do not live past the age of 5 because of a lung infection. There are also some children who live to adulthood.
Left lung defect is more common than right lung defect, but the mortality rate due to right lung defect is higher. The thoracic cavity of children with a defect in which one lung is missing is still completely normal. As the baby grows, the shape of the chest will gradually change. Specifically, the half of the thorax on the side without lungs will be flattened and the intercostal spaces will be narrowed.
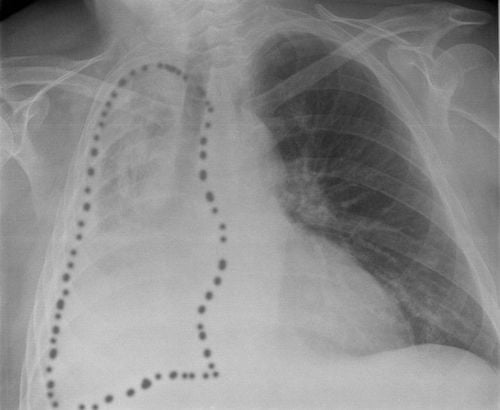
Clinically, children with one lung defect have no obvious symptoms. To diagnose a defect with one lung missing, measures such as chest x-ray, contrast bronchoscopy, and bronchoscopy can be applied.
Dị tật thiếu 1 bên phổi
1.3 Congenital emphysema Congenital pulmonary emphysema is also known as obstructive emphysema, hypertrophic emphysema, giant emphysema,... Based on changes in histology, emphysema Congenital lung disease is caused by incomplete development of lung parenchyma. Specifically, lung tissue with fibrous dysplasia, lacks elastic fibers, so it expands while the patient breathes in and cannot contract during expiration.
Congenital emphysema is common in the left upper lobe of the lung, rarely in the entire lung. The clinical signs of the disease often appear early in the first days of life: dyspnea on expiration, cyanosis, dry cough, when coughing, there is a whine in the lungs. Diagnostic tests to confirm congenital emphysema include: X-ray, contrast bronchogram.
Note, it is necessary to differentiate congenital pulmonary emphysema from pneumothorax, acquired emphysema (due to aspiration of foreign bodies causing bronchial obstruction), spontaneous pneumothorax or diaphragmatic hernia. Congenital emphysema has a rapid progression, if not treated promptly, the child can die. The treatment is to remove the lobe of the lung affected by emphysema.
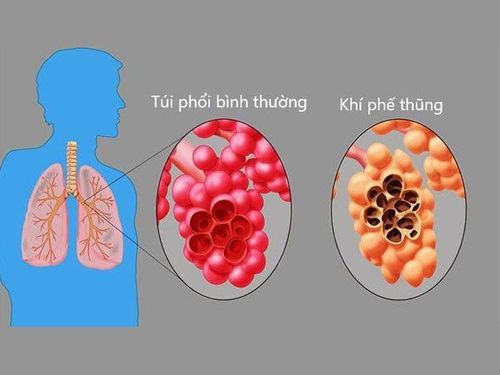
Khí thũng phổi
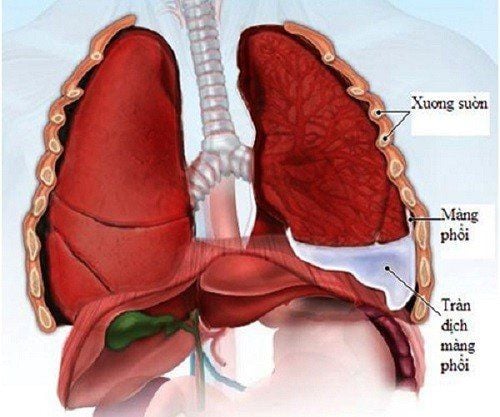
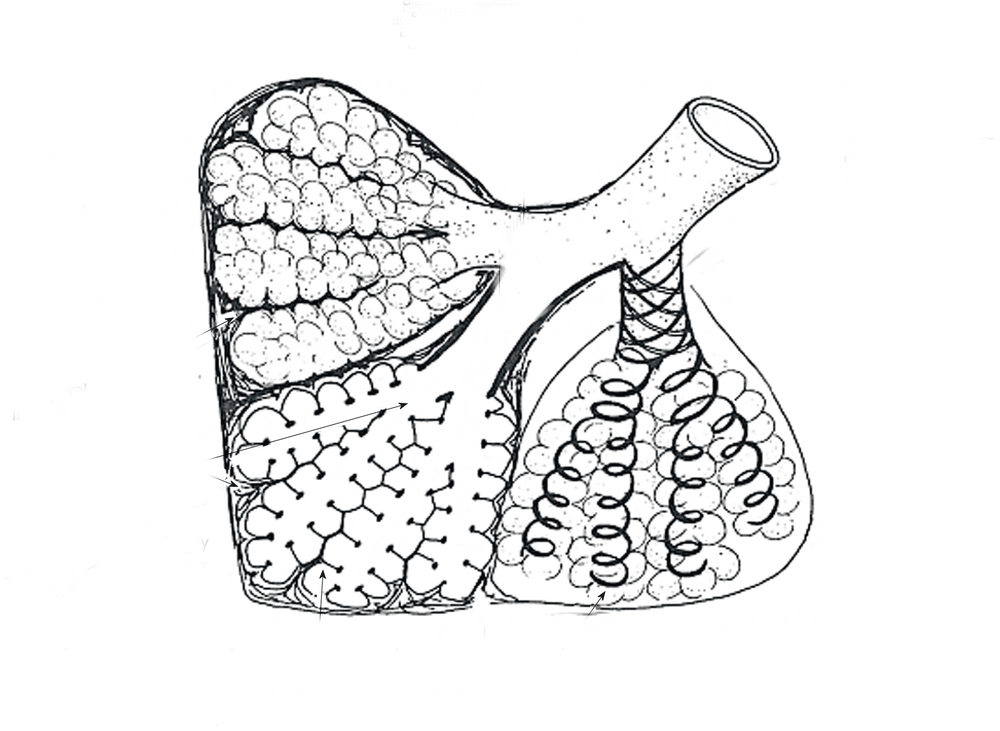
1.4 Hypoplastic Lungs Hypoplasia of both lungs is very rare malformation, not clinically significant because children with this defect are often not able to live. Pulmonary hypoplasia is common in the left lung, especially in the lower lobe. The size of the hypoplastic lung is small, dense, gas-free, the bronchi are dilated, with polyps, containing mucus and granular organization. The alveolar tissue of the hypoplastic lung is degraded or transformed into scar tissue, small bronchi and blood vessels are occluded.
Clinically, pulmonary hypoplasia usually appears from childhood. When the disease worsens, symptoms include cough, cough accompanied by purulent sputum, fever. Diagnosis of the disease is based on X-ray and contrast bronchoscopy.
Cases with hypoplastic lungs need to be operated on soon, should not wait until there are clinical symptoms to treat. Surgical removal of the lung tissue that has lost function will help avoid the risk of pneumonia in the lungs as well as other complications.
Hypoplastic lung malformation associated with congenital diaphragmatic hernia is a serious malformation, visceral organs from the lower abdomen can herniate into the pleural space, causing pressure on the lungs and mediastinum. In this case, the lungs are susceptible to infection, so early surgical intervention is required.
Recommended video:
Neonatal diaphragmatic hernia surgery at Vinmec - Save the life of infants with very severe diaphragmatic hernia
Most of the patients with hypoplastic lung malformations with diaphragmatic hernia die, so it is necessary to have surgery quickly to treat the diaphragmatic hernia and help the lungs expand after sealing the diaphragmatic hernia. . If surgery is delayed, the results will be poor because the lungs have been changed in morphology and cannot expand anymore. The best surgery for this case is 2 weeks after the baby is born.
Phổi giảm sản bẩm sinh
1.5 Abnormalities of the interlobar fissure Abnormalities of the interlobar fissure are a common congenital anomaly in the lungs but do not affect the health of the patient. Abnormalities of the interlobar fissure include: right upper and middle lobes fused together incompletely or completely (no fissure).
1.6 Auxiliary lungs The accessory lung is one of the congenital lung diseases, which is a lung organization that develops in the thorax, abdomen, neck, mediastinum and is independent of the main lung. It is important to pay attention to the subtype of lung called isolated lung, known by a number of names such as congenital bronchiectasis, ectopic lung lobe, congenital bronchopulmonary cyst,...
Isolated lung is common in left lung, in the posterior basal lobe, rarely in the upper lobe. This accessory lung resembles a cyst, which can be an independent cyst or multiple cysts. The isolated lung is fed by one or more malformed arteries. Isolated lungs can be located outside the lung parenchyma, completely isolated from the lung, or located in the pleural space, in the abdominal cavity, in the pericardium, or in the diaphragm. Congenital accessory lung defects are often accompanied by other malformations such as diaphragmatic hernia, esophageal cyst, pneumothorax, and absence of pericardium.
Although it is a congenital disease, the clinical symptoms of secondary lung often appear quite late, in young age or middle age, even in old age. Clinical symptoms of the disease usually appear when the size of the lung cyst changes or when the lung cyst has complications such as purulent inflammation or pneumonia. Symptoms depend on the stage of the disease. Specifically:
Stage 1: Before the lung cyst bursts into the trachea and causes purulent inflammation in the lung cyst: The patient presents with a dry cough, little mucus, shortness of breath, fatigue, and sweating a lot. Sometimes the disease develops into acute exacerbations with symptoms of fever, elevated temperature resembling pneumonia. There are also cases where there are no symptoms; Stage 2: After developing purulent inflammation, communicating with the bronchial tree: The patient coughs a lot, produces pus-filled sputum, fatigue, chest pain, shortness of breath and has acute episodes with high fever, increased sputum secretion. ; Stage 3: Developing purulent inflammation into the surrounding lung parenchyma, causing lung fibrosis and bronchiectasis: Symptoms are similar to stage 2. When chronic purulent inflammation occurs, the lungs become inflamed, bronchiectasis, and bronchiectasis. secondary, may have clubbing fingers.
Phổi phụ
Diagnosis of disease: In stage 1, X-rays can be taken to identify the disease. In stage 2, contrast angiography is needed to accurately diagnose isolated lung. At the same time, it is necessary to pay attention to the differential diagnosis of secondary lung with chronic lung abscess, cavernous tuberculosis, and bronchiectasis.
Secondary lung malformation can complicate pulmonary cyst rupture leading to spontaneous pneumothorax. The best treatment option is surgery, especially when complications are present. The basic surgery is to remove the isolated lung and the affected part of the lung. Cases of isolated lung that stick and invade healthy lung tissue often need to be cut along with the lobe if this lobe has complications of bronchiectasis.
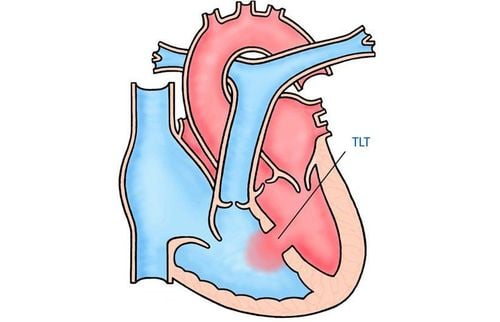
1.7 Aneurysm - pulmonary vein This is a rare malformation, known by many different terms such as: congenital pulmonary artery - vein, pulmonary varices, cavernous pulmonary hemangioma,...
Origin The cause of this condition is the widespread, abnormal development of the circulatory system of the blood vessels in the lungs. Common symptoms of patients are: rapid fatigue, shortness of breath that increases with heavy work, dizziness, headache, ringing in the ears, coughing a lot, may cough up blood, pale skin when doing heavy work, club fingers. drum,...
Diagnosis of aneurysms - pulmonary veins based on blood tests, X-rays. It is necessary to make a differential diagnosis with erythrocytosis and congenital heart defects.
The disease can lead to serious complications such as: rupture of aneurysms - veins causing bleeding into the bronchial tree or pleural cavity; cerebral circulatory disorders because blood clots block blood vessels in the brain; septic endocarditis; brain abscess. The only treatment for this condition is surgical removal of the arteriovenous aneurysm along with a lobe or lobe of the lung.
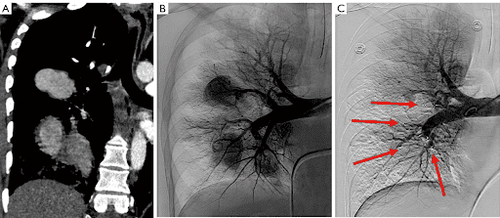
Phình động - tĩnh mạch phổi
2. Congenital bronchopulmonary malformations
2.1 Simple tracheobronchitis Simple tracheobronchitis is a rare congenital tracheal disease. Tracheal malformations associated with congenital bronchiectasis are common.
2.2 Aneurysm with limited wall of the trachea This birth defect is common in the cervical trachea. The patient presents with cough, accompanied by sputum, hemoptysis. Meanwhile, there are some cases without clinical symptoms. When diagnosing aneurysms that are confined to the wall of the trachea, the differential diagnosis should be made with goiter, medial and lateral cervical cysts. The treatment for this tracheal birth defect is to remove the bulge and reshape the trachea wall.
2.3 Bronchial diverticulum A common congenital bronchial disease is bronchial diverticulum. Bronchial diverticulum is usually localized to the medial bronchial wall and has many different morphologies. The typical clinical symptom is that the patient often coughs a lot, can cough up blood, and spits up bloody sputum. Attention should be paid to differential diagnosis of bronchial diverticulum from broncho-oesophageal fistula. In the case of complicated bronchial diverticulum, surgical removal of the diverticulum is required.
2.4 Main bronchus arising from the esophagus This is a rare form of anastomosis of the bronchopulmonary and anterior intestine. This is a case where the main bronchus is abnormally connected to the esophagus instead of the trachea. This malformation is usually detected in young children and older children, rarely in infancy. Bronchial malformations originating from the esophagus are often accompanied by other malformations: pulmonary hypoplasia, congenital heart disease, spinal malformations, gastrointestinal malformations, abnormalities in the kidneys, ribs, ... Accompanying malformations are the main cause of patient death.
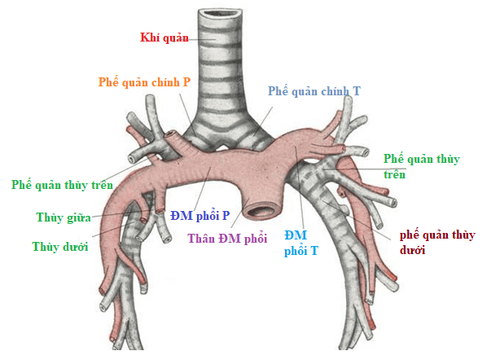
Động - tĩnh mạch phế quản
Signs of disease are: recurrent lower respiratory tract infections, early respiratory failure in young children unresponsive to treatment, severe atelectasis after esophagogastric fistula with tracheoesophageal fistula, chronic cough worsening when eating, pneumonia,... Diagnosis is based on X-ray methods, contrast esophageal X-ray, chest CT with reconstruction, bronchoscopy, esophagus .
The treatment method for bronchial malformations originating from the esophagus is surgery to remove the abnormal lung or lobe, re-insert the abnormal bronchus into the tracheobronchial tree in case the lung tissue is not severely damaged and the supply Blood supply to the bronchi - abnormally abundant lungs.
2.5 Tracheoesophageal fistula Tracheoesophageal fistula is a malformation that rarely exists alone, often in combination with other congenital malformations such as stricture of the esophagus, underdevelopment of the esophagus, .. When there is a tracheoesophageal fistula, the patient will inhale food or reflux from the stomach into the lungs, causing pneumonia, atelectasis,... If not diagnosed and treated promptly, the child will have Tracheoesophageal fistula can be fatal within the first day after birth.
Symptoms of tracheoesophageal - esophageal fistula accompanied by atrophy of the esophagus are: the nose and mouth of the child secrete a lot of yellow foamy mucus, shortness of breath, cyanosis, arrhythmia, lung moans, ... If there is a fistula of the upper esophagus into the trachea, the baby has pneumonia because breast milk flows into the lungs during feeding. Diagnose the disease by esophageal scintigraphy.
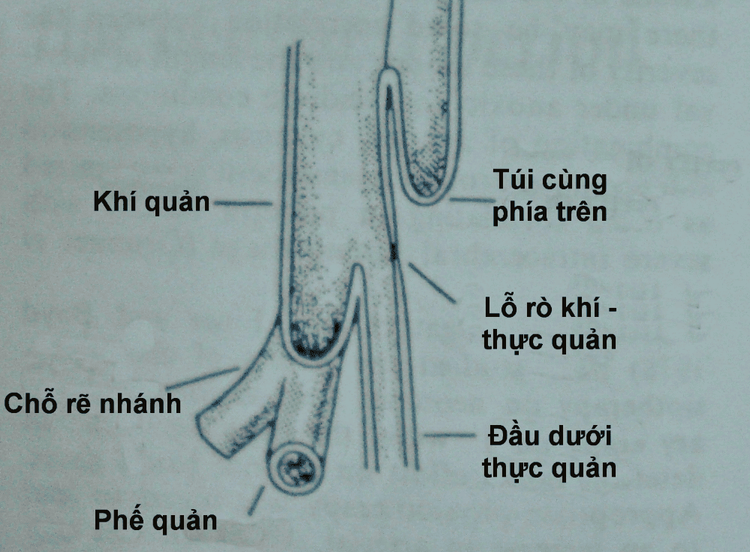
Vị trí dò khí phế quản - thực quản
Tracheobronchial fistula - esophagus is treated by surgery. Indications for caesarean section depend on the child's health status and it is recommended that surgery be performed soon after birth. Surgery is performed to remove the fistula between the esophagus and the trachea, connecting the atrophied esophagus for a long time. In case the oesophagus cannot be connected immediately, surgery is performed in 2 stages: stage 1 (separation of the esophageal-tracheal fistula, opening a gastrostomy to feed) and stage 2 (reconstruction of the esophagus by esophagitis). small intestine by the time the baby is 1 month old).
Congenital anomalies of the lungs, trachea, and bronchi need to be detected and treated early to minimize the risk of unpredictable complications that can be life-threatening.
If you have a need for consultation and examination at Vinmec Hospitals under the nationwide health system, please book an appointment on the website for service.
>> See more: Birth defects from statistics to causes – Article written by Doctor Do Phuoc Huy, Vinmec High Technology Center
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Recommended video:What is the job of the lungs?