This is an automatically translated article.
Optic neuritis is an inflammation that affects the myelin layer of the optic nerve, limiting the function of transmitting visual signals to the brain. Although the disease can sometimes fully recover after a while, an active examination and proper follow-up from the beginning is necessary to prevent complications of optic neuritis.
1. What is optic neuritis?
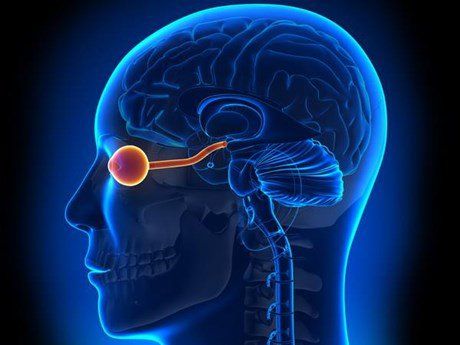
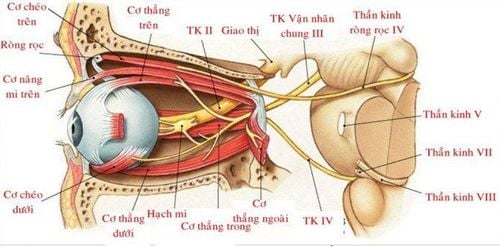
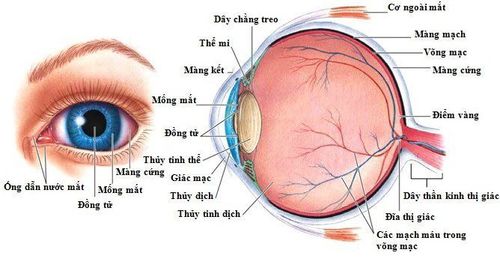
The two optic nerves are actually one nerve with axons originating from the ganglion cells of the retina at the back of the eye. These are the only nerves located entirely in the brain. The optic nerve carries visual information from the retina to the visual area in the occipital lobe of the brain for processing and analysis.
Optic neuritis is inflammation that damages the layer of myelin that covers the optic nerve. Common symptoms of optic neuritis include pain with eye movement and temporary loss of vision in one eye.
In some cases, the signs and symptoms of optic neuritis may be the first sign of multiple sclerosis or they may occur later in the course of the disease. . In addition, optic neuritis can also occur with conditions such as infections or immune diseases, such as lupus.
Fortunately, most people with an episode of optic neuritis eventually recover their vision without any specific treatment. Sometimes steroid medications can also speed up vision recovery after optic neuritis.

Dây thần kinh thị giác có vai trò rất quan trọng
2. What are the symptoms of optic neuritis?
Optic neuritis usually affects only one eye. Symptoms may include:
Pain: Most people with optic neuritis experience eye pain with movement of the eyeball. Sometimes the pain feels like a dull ache behind the eye. Loss of vision in one eye: Patients often seek medical attention because of a temporary loss of vision that occurs in one eye but presents with varying impairments. Significant vision loss usually develops over hours or days and will improve over weeks to months. However, a small number of people may experience permanent vision loss. Visual field loss: One-sided visual function may remain, but visual field areas may be affected, e.g. loss of central visual field, unilateral loss of visual field. Loss of color vision: In addition to the normal light perception function, optic neuritis also causes the patient to lose the ability to analyze colors. You may notice that colors appear less vivid than usual. Flickering light: Some people with optic neuritis report seeing bright lights that flash continuously or that flicker occurs only when there is eye movement.
Viêm dây thần kinh thị giác thường gây ảnh hưởng một bên mắt
3. What causes optic neuritis?
The exact cause of optic neuritis is still not well understood. This could be thought to be the result of the immune system misplaced attack on the myelin sheath covering your optic nerve, leading to inflammation and damage, and ultimately to vision loss, possibly temporarily or permanently.
Optic neuritis is often a sign of multiple sclerosis, a disease in which the immune system attacks the myelin sheath that covers nerve fibers in the brain and spinal cord, leading to inflammation and nerve damage. In this case, the optic neuritis usually goes away on its own, but it is easy to recur. Similarly, other autoimmune diseases, such as sarcoidosis, lupus... can also cause optic neuritis.
In addition, about half of the initial cases of optic neuritis are thought to range from an inflammatory response one week to one month after an upper respiratory viral infection. In addition, certain bacterial infections, including Lyme disease, cat scratch fever, and syphilis, as well as viral infections such as measles, mumps, herpes simplex, and herpes zoster... can also cause neuritis. visual meridians.
Certain drugs such as quinine, tetracycline, linezolid antibiotics, amiodarone, ethambutol and isoniazid... have shown evidence of involvement in the development of optic neuritis. Phosphodiesterase inhibitors such as Viagra can also cause optic nerve damage due to inadequate blood supply, leading to ischemia rather than primary inflammatory response.
On the other hand, there are also many conditions that can affect the optic nerve such as infection, trauma, genetics, toxic exposure, nutrition, damage to the optic nerve. Damage in diabetic vascular disease also affects the optic nerve. Therefore, the treatment of optic neuritis is directed at the root disease instead of treating the consequences.
Nguyên nhân gây ra viêm dây thần kinh thị giác vẫn chưa được xác định
4. How is optic neuritis diagnosed?
In addition to your symptoms, your doctor may diagnose optic neuritis with the following tests:
Myopia and assessment of your eye's response to bright direct light Visual examination Alphabetical force Ophthalmoscopy Cranial imaging with CT scan or MRI to rule out vision loss lesions in the brain

Chẩn đoán viêm dây thần kinh thị giác không quá khó
5. How is optic neuritis treated?
In some cases, you may not need treatment for optic neuritis. After a few weeks, the symptoms of this disease may go away on their own and vision will return to normal without leaving any sequelae.
Sometimes the doctor may also prescribe a short course of steroids. The drug will be used with a direct injection into a vein to achieve the highest anti-inflammatory effect, help the symptoms of the disease improve faster and minimize the inflammatory response. From there, optic nerve function will quickly be restored.
At the same time, it is important to actively seek and treat the cause of optic neuritis to limit the risk of recurrence leading to permanent damage.
6. What are the complications of optic neuritis?
Almost all cases of optic neuritis are completely reversible with no complications.
However, there are still a few cases of complications of optic neuritis, damage to the optic nerve, permanent or permanent loss of vision after an acute episode of inflammation. Without impaired vision, some people may also lose the ability to distinguish colors even though the inflammation of the optic nerve has gone into remission. In addition, the long-term use of corticosteroids in the treatment of optic neuritis can lead to significant side effects. It is associated with increased blood sugar, weight gain and osteoporosis... Despite this, given the benefits of short-term use of high-dose corticosteroids to control acute inflammation, this therapy is still favored in the treatment of patients. treatment of optic neuritis.
In addition, in individuals whose parenchymal lesions are detected by MRI, initial administration of intravenous steroids may help prevent future episodes of optic neuritis.
In a nutshell, optic neuritis is a condition affecting your eyes and vision that occurs when the optic nerve becomes inflamed. Patients will have symptoms of visual impairment in one eye and even pain when moving the eye.
Fortunately, most cases of optic neuritis go into complete remission on their own, leaving no serious complications. However, finding the cause and actively treating it is extremely necessary, in order to reduce the risk of recurrence as well as complications of permanent vision loss later on.
If you are experiencing vision problems, go to a medical facility immediately to be examined and treated by doctors as soon as possible. Currently, Vinmec International General Hospital has vision-related service packages such as:
Refractive error screening package Cataract surgery consultation and examination package Ortho-K package For more detailed information For details, you can contact Vinmec Health System nationwide, or register online HERE.
Reference source: medicinenet.com; hopkinsmedicine.org; mayoclinic.org
MORE:
Diagnosis and treatment of optic neuritis Optic neuritis: Causes, symptoms, complications Optic nerve atrophy: Causes, symptoms, diagnosis diagnosis and treatment