This is an automatically translated article.
The article is expertly consulted by MSc Vu Tan Phuc - Department of Medical Examination & Internal Medicine, Vinmec Phu Quoc International General Hospital.The incidence of liver disease and its complications is increasing rapidly. Prognosis is only meaningful when the patient is started with an intervention to treat compensated cirrhosis. Thus, an understanding of what compensated cirrhosis is, the causes of compensated cirrhosis and how to educate and prevent patients is essential, helping to delay the onset of serious complications later in life. .
1. What is compensated cirrhosis?
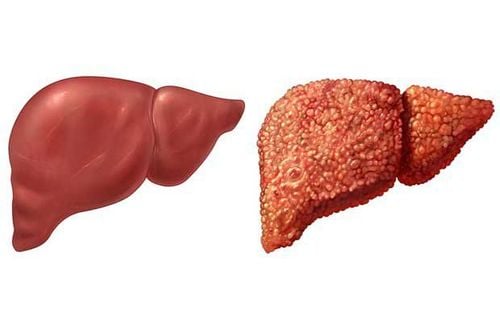
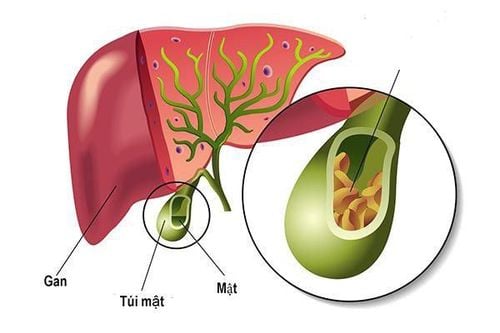
The liver is a large organ in the body, performing important functions such as detoxifying harmful substances in the body, cleaning the blood, and synthesizing nutrients. A liver injury of any cause can occur from any stage:Localized only in mild lesions Mild to moderate lesions, with signs of liver fibrosis already present moderate to severe liver fibrosis, cirrhosis but compensated cirrhosis Severe damage and liver failure, decompensated cirrhosis Cirrhosis is a local reaction in the liver parenchyma, occurring in response to cause liver damage. Each time the liver is damaged, a process of self-repair will occur and at the same time scar tissue will form. As cirrhosis progresses, more and more scar tissue forms, making it harder for the liver to function. When the patient is in the end stage, cirrhosis is when severe fibrosis occurs in the liver cells, causing loss of liver functions.
There are two types of cirrhosis described by the degree of residual liver function as compensated cirrhosis and decompensated cirrhosis. In which, compensated cirrhosis means the liver has scarred fibrosis but can still perform most of the basic functions to an acceptable level of the body. If the cause of continued liver damage is not ruled out, such as hepatitis C virus infection or alcohol consumption, etc., liver damage will continue to progress and the patient will begin to have more severe impairments in function. true liver function, transitioning to decompensated cirrhosis.
Tests can help determine the extent or stage of liver damage, from acute injury, fibrosis to true cirrhosis, and help monitor the patient's liver function. To do so, patients need to be monitored with tests and regular check-ups by liver disease specialists so that they can proactively treat and take care of them before symptoms occur.
Prognosis and survival in patients with compensated cirrhosis are markedly better in patients with compensated cirrhosis than in those with decompensated cirrhosis. In addition, the rate of complications related to cirrhosis is also lower and the possibility of having a liver transplant is also higher.

2. Causes of compensated cirrhosis
The causes of compensated cirrhosis are similar to the causes of cirrhosis in general, including diseases and conditions that can damage the liver parenchyma, impaired liver function:Excessive and prolonged alcohol abuse Long-term chronic viral hepatitis (hepatitis B, C and D) Having a large amount of fat in the liver (non-alcoholic fatty liver disease) There is a buildup of iron in the body (hemochromatosis) There is a buildup Copper in the body (Wilson's disease) Multiple cystic fibrosis alpha-1 antitrypsin deficiency Inherited disorder of sugar metabolism (galactosemia or glycogen storage disease) Hereditary digestive disorder (Alagille syndrome) Systemic liver disease the body's immune system (autoimmune hepatitis) bile duct hypoplasia Destroying the bile ducts (primary biliary cirrhosis) Hardening and scarring on the bile ducts (primary sclerosing cholangitis) Infections, such as syphilis or brucellosis Using medicines, such as methotrexate or isoniazid In addition, a person has an increased risk of cirrhosis if one or more of these risk factors are present. The risks are as follows:
Drinking too much alcohol: Excessive alcohol consumption is a risk factor for cirrhosis. Being overweight: Obesity increases the risk of conditions that can lead to cirrhosis, such as nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Viral hepatitis: Not everyone with chronic hepatitis will develop cirrhosis, but it is one of the leading causes of liver disease.

3. How are symptoms of cirrhosis compensated?
Patients with compensated cirrhosis can still live for many years completely unaware of liver damage with little or no symptoms. In fact, not all patients with compensated cirrhosis experience these symptoms but the common symptoms that may be experienced by this condition are:Itching Fatigue Loss of appetite Stomach pain Weight loss Plaque bruising of the skin Leg swelling or fluid retention in the abdomen Consciousness disorders Muscle atrophy In addition, patients with compensated cirrhosis also have a higher risk of liver cancer than the general population and may be similar to those with cirrhosis decompensation. Therefore, regular ultrasound and cancer markers are recommended to monitor the possibility of malignancy in the liver, because if detected early, the prognosis can be life-saving.
4. Aspects to note in the treatment of patients with compensated cirrhosis
Prevention of HCC is also an important part of the treatment of compensated cirrhosis. The reason is that the earlier it is detected, the greater the survival rate. Accordingly, the annual incidence of liver cancer will depend on the cause of the liver disease and the severity of the disease. To follow up, your doctor will need to order every 6 months with an abdominal ultrasound and a blood test for a-fetoprotein (AFP). In case the image obtained on ultrasound is not enough, the patient can be further evaluated with computed tomography or magnetic resonance imaging.
Non-drug measures to protect the liver and reduce the risk of progression of cirrhosis:
Regularly visit a hepatologist to check and monitor liver damage and liver function. Don't drink alcohol. Alcohol further damages liver cells and can accelerate liver fibrosis, causing compensated cirrhosis to rapidly turn into decompensated cirrhosis. Do not smoke or be exposed to chemicals or drugs that are harmful to the liver. Follow a healthy diet. Prioritize the use of plant-based foods by increasing the variety of fruits and vegetables. Choose whole grains and lean protein sources. Reduce the amount of fat and fried foods. Maintain the habit of drinking coffee. Caffeine may protect the liver against fibrosis and liver cancer. Maintain a healthy weight: Excess body fat can damage the liver. Counseling at nutritionists about a weight loss plan if you are obese or overweight. Reducing the risk of hepatitis: Sharing needles and having unprotected sex can increase your risk of getting hepatitis B and C. Hepatitis A and B vaccines are recommended, but there is currently no available vaccine for hepatitis C.
5. What is the prognosis of compensated cirrhosis?

The etiology of liver disease is an important factor in prognosis. Alcoholic cirrhosis usually has a worse prognosis if the patient continues to drink alcohol after the diagnosis has been made. Among patients with cirrhosis due to chronic hepatitis C, some studies show that more than 90% of patients are still alive at 5 years and but after 10 years only 70%.
However, in general, many patients with compensated cirrhosis can still have a relatively long life expectancy, comparable to that of the average person if detected early and followed well. With proper follow-up and prevention strategies implemented, the quality of life of patients with compensated cirrhosis is maintained and many of the serious complications associated with cirrhosis are delayed or prevented.
The danger of liver cancer has shown the importance of screening and early detection of the disease. Therefore, Vinmec International General Hospital has provided customers with a package of screening and early detection of liver cancer to screen for liver cancer for people at high risk of diseases such as: alcoholics, cirrhosis, family history of liver cancer, cirrhosis, hepatitis B virus infection, chronic hepatitis C,...
Service selection Package for screening and early detection of liver cancer, patients will be examined, consulted and performed tests, diagnostic imaging to evaluate liver function, liver diseases and liver cancer screening. With a system of modern machinery and a team of highly qualified and experienced doctors, Vinmec is committed to the best protection for the health of patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.