This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Ho Quoc Tuan - Anesthesiologist - General Surgery Department - Vinmec Nha Trang International General Hospital.Uterine malformation is an abnormality in the female reproductive organs that requires surgical intervention. In particular, spinal anesthesia combined with epidural can be performed with simple surgery and requires moderate muscle relaxation.
1. What is uterine malformation?
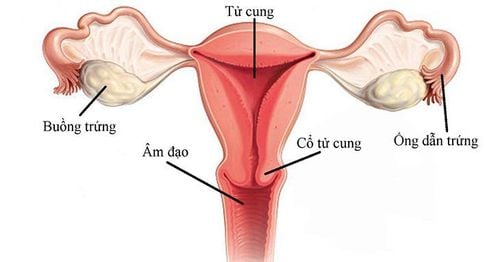
The uterus is one of the female reproductive organs. Abnormalities in the uterus, also known as uterine malformations, can affect fertility as well as labor.There are many types of uterine abnormalities including:
No uterus: Women will not have periods and cannot become pregnant. Double uterus: There are two uteruses in the pelvis and share a vagina. A woman can still get pregnant if the function of one of the uteruses is normal. Separated uterus: This is the most common type of malformation, and will make it difficult to conceive. Unicornuate uterus: The uterus has only one ovary and one fallopian tube, so it can be difficult for a woman to get pregnant. Baby uterus: In this case, the uterus is underdeveloped, the size of an adult's uterus is only equal to that of girls. These women usually don't have ovaries, so they can't get pregnant. Uterine malformations can affect reproductive health. Therefore, if detected early, abnormal signs need to be examined and monitored to limit adverse effects on health.

Dị dạng tử cung có thể gây ảnh hưởng đến sức khỏe sinh sản
2. Spinal anesthesia combined with epidural anesthesia in uterine malformation surgery
2.1 Combined spinal - epidural Anesthesia Combined spinal - epidural analgesia is a new anesthetic technique that can be applied to a wide range of patients of different ages. This is a combination of anesthetic techniques with the aim of achieving the most ideal anesthesia conditions for the patient.Spinal anesthesia combined with epidural analgesia can be performed for simple surgeries. Uterine malformation surgery is a type of surgery below the navel and has moderate muscle relaxation, so it is possible to apply combined spinal-epidural anesthesia.
2.2 Indications and contraindications Indications for combined spinal and epidural anesthesia for uterine malformation surgery.
Contraindicated in the following cases:
Allergy to local anesthetic Inflammation of the needle puncture site Lack of adequate circulating volume, shock Severe coagulopathy Insufficient anticoagulation time stopped Valve stenosis Closed leaflets, tight aortic valve Increased intracranial pressure 2.3 Procedures Step 1: Preparation
The person performing the combined spinal-epidural anesthesia is an anesthesiologist. Some tools to prepare include:
Spinal needles, pre-packed epidural anesthetic kits Sterile towels, hand towels, cups of antiseptic solution, surgical forceps Syringes syringes of all kinds Adhesive bandages sterile waterproof back patch Sterile gloves and clean gloves Anesthesia machine, aspirator, and intubation luminaires, tracheal tubes with balloon inserts of different sizes Betadine antiseptic Solution Medications used include include:
Bupivacaine, levobupivacaine Fentanyl 2ml Morphine Infusion: ringer lactate, ringerfundin Vasopressors: ephedrine tube 30mg/ml Atropin sulphate Anti-shock box Before surgery, the patient will be explained the purpose by the medical staff. , analgesia technique so that the patient knows and cooperates.
Trước khi tiến hành phẫu thuật, người bệnh sẽ được nhân viên y tế giải thích cặn kẽ về các vấn đề liên quan như mục đích, kỹ thuật vô cảm
Conduct an intravenous line in the hand with a needle 18, intravenously infuse 300 - 500 ml of Ringer lactate solution before anesthesia. Continuous monitoring of indicators: pulse, blood pressure, capillary oxygen saturation, respiratory rate. Place the patient in an anesthetic position: sitting or lying position, bending the shrimp's back Determine the position of the anesthetic needle (the horizontal line passes through the two iliac crests corresponding to L4-L5). Disinfect the back area with 10% Betadin solution. x Sterile towel with holes in the back area. Wipe Betadin from the area to be numbed with sterile gauze. Conduct spinal anesthesia:
27G spinal anesthetic needle puncture, at position L2 - L3 or L3 - L4, the bevel of the needle is parallel to the body. A feeling of loss of resistance can be felt when the needle passes through the yellow ligament and dura, when withdrawing the needle barrel and seeing cerebrospinal fluid flowing out of the needle shank, the needle is in the correct position. Conduct injection of anesthetic solution into the subarachnoid space, slow speed. Commonly used anesthetic solutions are: Bupivacaine 0.1-0.15 mcg/kg Fentanyl 25-50 mcg, can be combined with 100mcg morphine to relieve postoperative pain. After the anesthetic is injected, check to see if the cerebrospinal fluid is easily aspirated, indicating that all the anesthetic solution has been injected into the subarachnoid space. Withdraw the anesthetic needle and seal the puncture with waterproof tape. Put the patient in supine position, breathe oxygen, increase the infusion rate, continuously monitor arterial blood pressure every 2 minutes. Monitor the degree of sensory block by pricking the skin with a blunt needle. Monitor the degree of motor block using the Bromage scale. Surgery can be initiated when the degree of sensory block reaches T10. When blood pressure decreases > 20% compared with the patient's baseline blood pressure, administer intravenous 10-30 mg of Ephedrine. Intravenous 0.5 mg Atropin when heart rate decreases by more than 20% of the patient's baseline heart rate, may be repeated after 5-10 minutes if response is poor, to a maximum of 3 mg. Monitor recovery in the recovery room, the recovery of movement of the legs and vital signs, side effects of anesthetics, anesthesia complications and surgical complications. Epidural Anesthesia:
Anesthetize the Tuohy needle puncture site with Lidocaine. Determine whether the Tuohy needle has entered the epidural space by using a non-resistive technique with a syringe filled with fluid (normal saline NaCl 0.9%). Check for blood or cerebrospinal fluid reflux into the needle shaft. Insert the catheter toward the patient's head and place the catheter 4-5 cm in the epidural space (5 cm in obese patients). In case of difficult catheterization, the catheter should never be removed alone, but both the catheter and the Tuohy needle must be removed to avoid the risk of catheter rupture in the epidural space. Withdraw needle Tuohy. Suction through the catheter to check for bleeding. Connect the bacterial filter to the outer end of the catheter. Test dose: inject 2-3 ml of 2% lidocaine mixed with adrenaline. Look for symptoms of catheter entering the subarachnoid space (sudden motor block, similar to spinal anesthesia...) or symptoms of catheter entering blood vessels (metallic taste in the mouth, tinnitus, tinnitus sensation). , dizzy ...). Secure the catheter with clear tape. After the test dose 5 minutes: inject another 15-20 ml of Lidocaine 2% in combination with 50-100 mcg of Fentanyl. Put the patient in supine position, breathe oxygen, increase the infusion rate, continuously monitor arterial blood pressure every 2 minutes. Monitor the degree of sensory block by pricking the skin with a blunt needle. Monitor the degree of motor block using the Bromage scale. Surgery can be initiated when the degree of sensory block reaches T10. When blood pressure decreases > 20% compared with the patient's baseline blood pressure, administer 10-30 mg of Ephedrine intravenously. Intravenous 0.5 mg Atropin when heart rate falls by more than 20% from the patient's baseline heart rate. Intraoperative epidural anesthesia is used to relieve postoperative pain when the spinal anesthesia wears off, usually 3 hours after surgery or as soon as the patient has pain with a VAS score > 4, titrate the analgesic dose and maintain with Electric syringe pump 3-5 days after surgery. Analgesics: Bupivacaine 0.1% solution + Fentanyl 1mcg/ml, analgesic titration to maintain VAS score < 4. 2.3 Monitoring and management of complications After surgery, patients should be monitored for signs survival such as pulse, temperature, blood pressure, breathing rate,... In addition, during and after anesthesia the patient may experience some complications such as:

Đau đầu hay tụt huyết áp là một số biến chứng có thể gặp phải sau khi thực hiện thủ thuật
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
Doctor Quoc Tuan has many years of experience in the field of Anesthesiology - resuscitation at Hoan My Danang Hospital and Phu Yen Provincial General Hospital before being an Anesthesiologist and resuscitator at the Operating Room - Department of Medicine. General surgery of Vinmec Nha Trang International General Hospital as it is today.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
SEE MORE
Female infertility due to uterine abnormalities Things you may not know about the uterus What is a double uterus?