This is an automatically translated article.
Posted by Specialist II Khuc Thi Nhan - Neurologist - Outpatient Department - Vinmec Times City International Hospital
Peripheral cold-induced facial paralysis (cold-induced peripheral palsy or Bell's facial palsy) is a fairly common disease, accounting for about 70% of peripheral nerve palsy, some cases familial. The disease occurs in both sexes and at any age, but mainly in the age group of 20-40. The annual incidence is about 20 cases per 100,000 population.
1. What is peripheral facial paralysis due to cold?
Peripheral facial paralysis is paralysis of all muscles on one side of the face, including the upper and lower face. The disease develops suddenly, often following a cold or viral infection (herpes simplex virus type I, which causes cold sores on the lips, and herpes zoster virus, which causes shingles and chickenpox). Facial paralysis is secondary to facial neuritis (bulging, edematous, and compressed nerve in the inner ear canal). The disease usually appears at night, occurs suddenly after the mastoid pain (behind the ear). When the patient wakes up, the patient's eyes on the paralyzed side do not close tightly, the median nucleus deviates to the opposite side (the healthy side), reduces or loses forehead wrinkles and nasolabial folds on the paralyzed side, and at the same time reduces tear secretion, reduces sensation in the brain. area of the external ear canal as well as decreased taste in the anterior 2/3 of the tongue on the paralyzed side. After 2-3 days, some cases appear blisters in the area of the external ear canal (Ramsay-Hunt area). Cold peripheral facial paralysis is usually simple, not associated with other neurological damage.
This is a non-life-threatening disease, but about 20% of cases leave sequelae of spastic facial paralysis affecting aesthetics (especially in young women), corneal ulcers on the left side of the eye, syndrome "Crocodile" tears show increased tear secretion when eating. However, if diagnosed early and treated promptly, properly can reduce the rate as well as the degree of sequelae.
2. What causes Bell's facial paralysis?
The exact cause of Bell's palsy is unknown, but most researchers believe it's possible that a viral infection (herpes simplex virus or herpes zoster) causes swelling and inflammation of the facial nerve. (VII nerve).
Herpes simplex type I: a common virus that causes cold sores on the lips, present in many cases of Bell's facial paralysis but has not yet been shown to have a direct link between Bell's palsy and the virus. Herpes zoster virus: causes shingles and chickenpox. Some cases of facial paralysis a few days after facial paralysis appear blisters in the outer ear canal, but most of the cases are not unusual, but experts still believe that the herpes zoster virus is the cause of some cases of paralysis. Bell's because the virus hides in nerve roots (this hypothesis is disputed).

Hình ảnh mụn nước ở vùng ống tai ngoài (vùng Ramsay-Hunt)
3. Risk of peripheral facial paralysis due to cold?
Some people are more at risk of Bell's palsy than others. The risk is higher in people with diabetes, pregnancy (in the last 3 months or the first week after giving birth), colds or flu, measles, mumps, herpes (Herpes simplex type I), and chickenpox. chicken pox and shingles (Herpes zoster), family history of facial paralysis...
4. Diagnosis of peripheral facial paralysis due to cold
For a definitive diagnosis based on clinical symptoms, computed tomography or cranial magnetic resonance imaging is not necessary. As for the differential diagnosis, Bell's palsy must be differentiated from Lyme disease, Guillain-Barré syndrome, sarcoidosis, parotid adenoma, and stroke. Lymphoma can also cause facial paralysis (rare).
5. Methods of treatment of peripheral facial paralysis due to cold
Currently for the treatment of peripheral cold-induced facial paralysis, including drug therapy, rehabilitation physiotherapy and combined acupuncture.
5.1 Drug therapy Some of the following drugs are prescribed by the doctor in treatment, including:
Corticosteroids (Prednisolone): The dose is 1 mg/kg/day x 3 days for the first time, then gradually decreased (reduced by 10 mg). every 3 days) then cut. The drug is usually taken within 15 days. Contraindicated in people with hypersensitivity to the drug. With caution in the presence of osteoporosis, peptic ulcer disease, diabetes, hypertension, heart failure, growing children. Undesirable effects can be insomnia, nervous excitability, cataracts, glaucoma, edema, hypertension, pancreatitis, peptic ulcer. Antiviral drugs (Acyclovir, Famyclovir...): 200mg, 400mg, 800mg tablets. Dose 800mg x 5 times / day, each time 4 hours apart. Duration of treatment is from 5-7 days, used as soon as the infection or when the blisters appear. Contraindicated in case of hypersensitivity to the drug. Undesirable effects such as nausea, vomiting, diarrhea, abdominal pain headache. Use caution during pregnancy and lactation. Research results in European and American countries show that the combination treatment with corticosteroids and anti-herpes drugs has better results than the treatment with corticosteroids alone.
B vitamins (B1, B6, B12): have the effect of promoting the recovery of damaged nerves such as increasing the synthesis of nucleic acids and proteins in nerve cells, increasing the synthesis of Lecithin (an important component of Myelin sheath) Medicines to regenerate and restore Myelin sheath: Cytidine-5 disodium-monophosphate ... Eye care and protection: daily eye drops with artificial tears, wear eye protection during the day to prevent foreign objects entering Eye causes inflammation of the cornea, sclera, and conjunctiva. Use hypoallergenic tape over your eyelids to aid blinking during the day and close at night and prevent inversion.
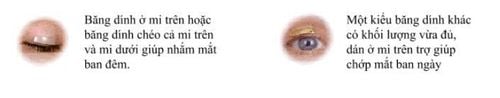
Người bệnh có thể dùng bằng dính chăm sóc và bảo vệ mắt theo hướng dẫn
5.2 Physical therapy and rehabilitation methods Along with the use of drugs, physical therapy and rehabilitation play an important role in helping to achieve high results in the treatment and prevention of hemifacial spastic complications, face synchrony (appears mass winking when smiling). Rehabilitation should begin within the first week of illness.
For cases of hemifacial spasticity or facial spasm that affects aesthetics, Toxin Botulinum can be used topically to reduce spasticity.
5.3 Combined acupuncture method Acupuncture can be performed after 7-10 days from the time of illness, if acupuncture is performed on the first day after paralysis, it can cause spasticity in the later half of the face.
Prophylactic treatment of Bell's facial palsy until now, there is no effective preventive treatment. Therefore, patients should take the initiative to avoid affecting their health and losing confidence in life.
Neurology Specialist - Vinmec International General Hospital currently receives and treats patients with facial nerve paralysis due to many causes. The hospital currently has a team of experienced and well-trained specialists, especially with a system of modern equipment, meeting international standards, and professional service quality to bring effective diagnosis and treatment. high, minimizing complications for the patient.
Therefore, Vinmec hospital is now a prestigious health care center for all types of customers who can visit when having any health problems.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Ropper AH, Brown RH. Facial palsy. Print: Allan H. Ropper, Robert H. Brown, eds. Adams & Victor's principles of neurology. New York : McGrawHill, 2005;1181-5. Sullivan FM, et al. Early treatment with prednisolone or aciclovir in Bell's palsy. N Engl J Med 2007;357:1598.