This is an automatically translated article.
The article was professionally consulted by Pharmacist, Master Nguyen Hoang Phuong Khanh - Clinical Pharmacist - Faculty of Pharmacy - Vinmec Central Park International General Hospital.With the advent of antibiotics, the medical field of treating infectious diseases has turned a new page, thanks to antibiotics millions of lives have been saved from dangerous infections. So what are antibiotics? Mechanism of action of antibiotics?
1. Definition of antibiotic
Alexander Fleming (1881-1955) was a Scottish physician, biologist and pharmacologist. He is considered the one who ushered in the era of antibiotic use in medicine.Antibiotics are antibacterial substances produced by strains of microorganisms or of synthetic origin, which inhibit the growth and development or destroy other microorganisms.
2. Antibiotic classification
There are many ways to classify antibiotics, but the most common classification is by spectrum of action and by mechanism of action of antibiotics.
2.1 Classification by spectrum of action
Due to the specific mechanism of each antibiotic, each group only works on certain strains of bacteria. This limit is called the antibacterial spectrum of the antibiotic.
Narrow-spectrum antibiotics (selective antibiotics): Antibiotics only work on 1 or certain species of microorganisms. For example, isoniazid is only active against Mycobacterium tuberculosis. Broad-spectrum antibiotics: Antibiotics are active against a wide range of bacteria, both gram-negative and gram-positive, eg quinolones, macrolides, carbapenems. Improper use of broad-spectrum antibiotics can disrupt the body's resident flora and cause bacterial infections (eg, Clostridium difficile infection) following antibiotic use.
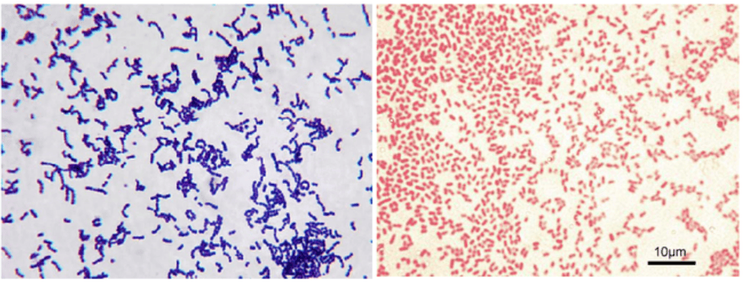
Hình ảnh vi khuẩn gram âm và gram dương
2.2 Classification according to chemical structure
Beta lactam group: Includes antibiotics with a chemical structure containing a Beta lactam ring, divided into four groups:
Penicillin: A derivative of 6 aminopenicillanic acid. Includes: benzylpenicillin, methicillin, amoxicillin, piperacillin etc. Penicillin has a spectrum on gram-negative and gram-positive. However, because bacteria have a resistance mechanism by secreting beta-lactamase enzymes, some antibiotics are combined with beta-lactamase inhibitors to increase the bactericidal effect such as amoxiciclin/clavuclanic acid; piperacillin/tazobactam. Cephalosporins: Composed of a beta lactam ring and a dihydrothiazine ring. Changing the substituents on the ring will lead to changes in the properties and biological effects of the antibiotic. Cephalosporins are divided into 4 generations. 1st generation: Acting mainly on Gram-positive: cefazolin, cefalexin Generation 2: Increasing spectrum of action on Gram-negative: cefuroxime, cefamandol, cefaclor, and active against anaerobic bacteria Bacteroides fraginalis: cefotetan, cefoxitin Generation 3: Strong effect on Gram-negative: cefotaxime, ceftriaxone, ceftazidime, cefixime. 4th generation: Broad spectrum on Gram-positive and Gram-negative, including Pseudomonas: cefepime. Generation 5: Including the spectrum on MRSA (Methicillin resistant staphylococcus aureus): ceftaroline Carbapenem: Because the drug has high affinity for PBP of gram-negative and gram-positive bacteria, along with a structure that is difficult to destroy by beta-lactamase enzymes, so this is the broadest spectrum of beta-lactam antibiotics, eg meropenem, imipenem-cilastatin, ertapenem. This is a group of "reserve" antibiotics, only used in cases of severe infections, multi-resistant infections. Monobactam: is a beta-lactam antibiotic, only active against gram-negative bacteria: Aztreonam Aminoglycoside group (amikacin, tobramycin, gentamycin): In chemical structure, it contains a sugar base (ose) and an amino functional group. named aminoglycosides. It is an antibiotic active against gram-negative bacteria, and a gram-positive agonist (gentamycin).

Tobramycin – Kháng sinh nhóm aminoglycosid
Macrolides: Isolated from Streptomyces. Common active ingredients are erythromycin, clarithromycin, azithromycin. This class of antibiotics has a spectrum on gram-negative, gram-positive and atypical bacteria.
Lincosamide group: This group includes two drugs, lincomycin and clindamycin. Clindamycin has a spectrum of activity mainly against gram-positive and anaerobic bacteria.
Quinolone group: Is a fully synthetic antibiotic. The first generation is nalidixic acid, the following generations are added fluorine to the ring, so it is named fluoroquinolone. For example: ciprofloxacin, levofloxacin, moxifloxacin. This is a group of antibiotics with strong effects on Gram-negatives such as Enterobacteriaceae, Haemophilus spp, Neisseria spp. In addition, ciprofloxacin and levofloxacin are also active against Pseudomonas aeruginosa.
Glycopeptide group (Vancomycin, Teicoplanin): this is a group of semi-synthetic antibiotics, with a spectrum of action on gram-positive, including resistant gram-positive strains. When used, these antibiotics need to be measured in the blood to ensure effective treatment and reduce nephrotoxicity.
Other groups:
Oxazolidone (linezolid) : is a fully synthetic antibiotic with strong gram-positive activity such as staphylococcal and streptococcal. In addition, the drug is also effective against multi-resistant gram-positive bacteria such as MRSA, VRE. Chloramphenicol (chloramphenicol, thiamphenicol). Since it has been used for a long time, the rate of drug resistance is high. Besides, the drug has serious toxicity on hematopoietic organs, causing marrow aplasia, causing severe anemia, so the drug is no longer used much in clinical practice. Tetracycline (tetracyclin, doxycyclin, minocyclin): An antibiotic with 4 hexagonal rings, isolated from Streptomyces Aureofaciens or semi-synthetic. The drug has a spectrum of action against gram-positive, gram-negative and intracellular bacteria. Do not use the drug for young children because the drug attaches strongly to bones and teeth causing growth retardation, tooth damage and tooth discoloration. Nitro-imidazol: Are antibiotics derived from chemical synthesis: metronidazole, tinidazole. The drug has a spectrum on unicellular and anaerobic bacteria such as Bacteroides, C.difficile, H.Pylori. Sulphonamide: Has bacteriostatic effect, not used alone. The drug has a spectrum on gram negative, gram positive, Actinomyces, Chlamydia, Plasmodium, Toxoplasma. Trimethoprime: often combined with sulphonamide to treat gram-negative and gram-positive infections, including multi-resistant bacteria such as: Acinetobacter, B.Cepacia, Stenotrophomonas maltophilia. Polymyxin (Polymyxin B, Colistin): An antibiotic synthesized from Bacillus polymyxa. After the advent of the aminoglycoside group, polymyxins were rarely used because of their high nephrotoxicity. However, with the emergence of many multidrug-resistant gram-negative bacteria, polymyxin was re-used to treat Acinetobacter spp, Pseudomonas spp. Group of antibiotics against tuberculosis: rifampicin, isoniazid, pyrazinamide, ethambutol.
3. Mechanism of action of antibiotics
3.1 Inhibition of bacterial cell wall biosynthetic enzymes involved in peptidoglycan splicing to form the bacterial wall.
With Gram-positive bacteria: Gram-positive bacteria do not have an outer cell membrane, so beta-lactams act directly on PBP. Glycopeptide group (Vancomycin) attached to D-alanyl-D-alanine, thereby affecting the synthesis of peptidoglycan.
3.2 Inhibition of the plasma membrane
The main function of the cytoplasmic membrane is to selectively permeate substances. When the antibiotic is attached to the membrane, it changes the selective permeability of the membrane, causing the ionic components inside to escape and water from the outside to enter, resulting in cell death.
Example: Polymyxin B, colistin attached to the cell membrane of gram-negative bacteria.
3.3 Inhibition of Protein Biosynthesis
Tetracycline: binds to the 30s subunit, prevents tRNA from binding to ribosomal mRNA, is a bacteriostatic antibiotic. Aminoglycoside: binds to the 30s subunit, prevents mRNA transcription, and at the same time causes mRNA to be transcribed incorrectly, is a bactericidal antibiotic. Macrolide, lincosamide: attach to the 50s subunit, end the development of the protein chain, is a bacteriostatic antibiotic. Chlorpheninramine: binds to the 50s subunit and prevents the binding of amino acids to form protein chains, is an bacteriostatic antibiotic. Linezolid: binds to 23S ribosomal RNA of the 50s subunit, preventing the formation of the 70s complex required for protein synthesis; is an bacteriostatic antibiotic. 3.4 Inhibition of Nucleic Acid Biosynthesis
Quinolone: acts on DNA gyrase enzymes and topoisomerase IV affects DNA replication. Rifampicin: binds to DNA-dependent RNA polymerase, inhibits RNA synthesis of bacterial cells 3.5 Inhibits folate biosynthesis:
Sulfonamide: the drug is structurally similar to PABA (para-aminobenzoic), so it competes with PABA It is a substance involved in the metabolism of folic acid (a precursor for nucleic acid synthesis), bacteriostatic effect. Trimethoprime: inhibits dihydrofolate reductase enzyme, affects folic acid synthesis, bacteriostatic effect.
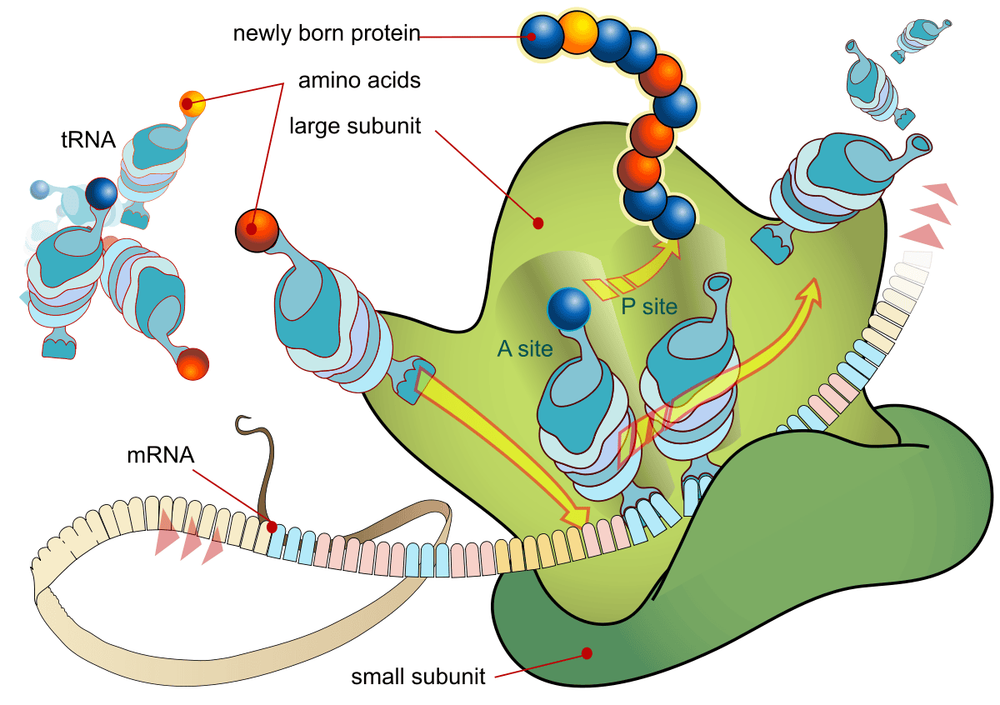
Sinh tổng hợp protein l
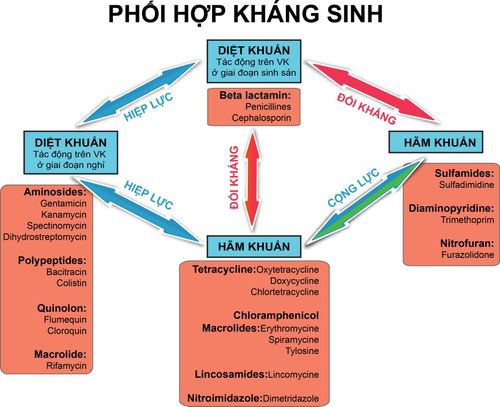
Thus, each resistance has a different mechanism, affecting the growth and development of bacteria. Antibiotic combination is also based on the site of action to increase the synergistic effect of antibiotics.
When choosing an antibiotic to treat a patient, the doctor will choose an antibiotic based on the infection status, the risk of multi-resistant bacteria, the location of the source of the infection, the antibacterial spectrum of the antibiotic, and the permeability of the antibiotic. antibiotics into infected tissue.
At Vinmec, antibiotics of the above groups are fully supplied, quality assurance, response to infection treatment. In addition, the hospital has also implemented an antibiotic use management program since 2017, with the close cooperation of doctors and clinical pharmacists to make a reasonable antibiotic choice, ensuring treatment effectiveness. , minimize drug side effects and limit the risk of antibiotic resistance.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.