This is an automatically translated article.
The article was written by Dr. BS Pham Thi Viet Huong - Doctor of Hematology - Oncology. Currently, Doctor Viet Huong is working at the Hematology and Cell Therapy Unit of the Center for Regenerative Medicine and Cell Therapy - Vinmec Times City International General Hospital.
Bone marrow cell leukemia or chronic myeloid leukemia (CML) is a rare cancer of the bone marrow - the spongy tissue inside the bones that makes blood cells.
1. What is chronic myeloid leukemia?
Each person's blood is composed of 3 main cell components: red blood cells, white blood cells and platelets. These blood cells all come from a common type of cell in the bone marrow, called "hematopoietic stem cells". They will grow, mature and perform special functions, then age, die, and be replaced by new cells. This process occurs in the body and is always strictly controlled.
However, in leukemia, things can go wrong when too many white blood cells are produced in the bone marrow, beyond the body's ability to control. In chronic myeloid leukemia, granulocytes proliferate uncontrollably, but these cells are still well differentiated, taking on a part of the body's functions. That's why chronic leukemia usually progresses more slowly and the symptoms aren't as intense as acute forms of leukemia.
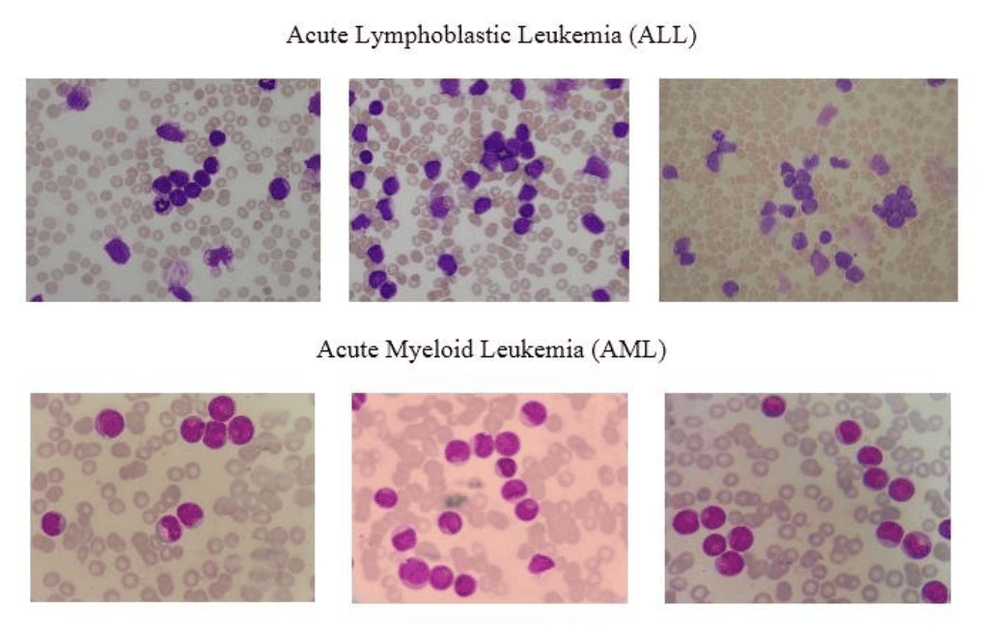
Bệnh bạch cầu cấp tính dòng tế bào Lympho (ALL)
Normally chromosomes contain DNA, which helps determine how a cell matures and develops. Chromosomal damage thus leads to changes in cell function and activity that cause chronic myeloid leukemia. The most characteristic change is on chromosomes 9 and 22.
For some reason, each chromosome will be cut apart and swap places. Finally formed a mutant chromosome with shorter size with 1 segment is chromosome 22 and 1 segment is chromosome 9. It is called the Philadelphia chromosome (or infection for short). Ph chromosome)
2. Causes of chronic myeloid leukemia
To date, it is not known exactly what causes the Philadelphia chromosome to form. Epidemiological studies have shown that it is possible that some people are exposed to high-intensity, prolonged exposure to chemicals or radiation, leading to chromosomal damage.
The formation of the Philadelphia chromosome also leads to a rearrangement of the corresponding DNA fragments located on that chromosome. Then a new gene is formed, called the BCR-ABL gene (consisting of the BCR gene segment of chromosome 22 attached to the ABL gene of chromosome 9).
This BCR-ABL gene promotes rapid, non-stop cell proliferation, but prevents white blood cells from aging and dying. This is the first germ to cause chronic myeloid leukemia.
3. Who can get chronic myeloid leukemia?
Bệnh bạch cầu mạn dòng tủy thường gặp nhất ở những người khoảng 60 tuổi trở lên
Chronic myeloid leukemia mainly occurs in adults, the most common average age is about 60 years old. The risk of the disease increases with age.
4. Symptoms of chronic myeloid leukemia
In the early stages, the cancer cells are still functional, patients often have no obvious symptoms, may only feel fatigue, and abdominal pain due to splenomegaly.
But later on, if not well controlled, the cell's ability to differentiate and function is increasingly affected. At that time, symptoms appear more pronounced, most commonly feeling short of breath, pale, night sweats, weight loss, poor cold tolerance and enlarged spleen occupying the entire abdomen.
In the final stage, the patient presents with 3 typical symptoms: paleness, hemorrhage and fever.
5. Diagnosis of chronic myeloid leukemia?
Xét nghiệm sinh hóa máu giúp chẩn đoán bệnh bạch cầu mạn dòng tủy
Take a complete and detailed medical history and the patient is examined in general to record the signs of the disease.
5.1 Conduct tests Total blood analysis Blood biochemistry (including liver and kidney function tests) Bone marrow aspiration to do specialized tests such as: myeloma, chromosomal and fluorescence hybridization techniques In situ optical imaging (FISH) to survey the Philadelphia chromosome, PCR to evaluate the BCR-ABL mutation gene There are also routine tests such as: coagulation, echocardiogram, electrocardiogram, chest X-ray, virus ... Bone marrow assessment is an important test and requires high technology, as well as requires experienced paraclinologists, so it is usually conducted at hospitals specializing in hematology and/or oncology. letters. After having the appropriate laboratory results along with the signs of the disease, the doctor will decide whether the patient really has chronic myeloid leukemia before proceeding with the appropriate treatment. 5.2 Differential diagnosis It is important to distinguish newly acquired chronic myeloid leukemia from reactive leukocytosis in infection, inflammation, or cancer.
6. Treatment of chronic myeloid leukemia?

Hình ảnh cấy ghép tủy xương để điều trị bệnh bạch cầu mãn tính dòng tủy
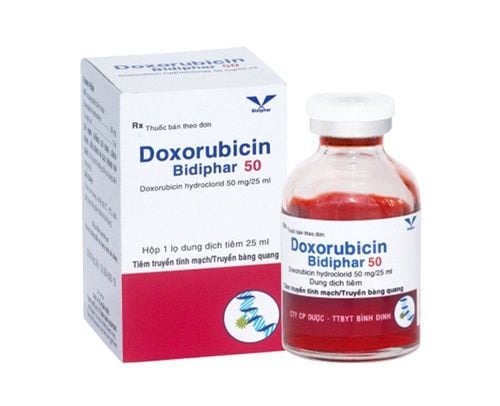
Hematologists and oncologists will treat you. Treatment includes medication or a bone marrow transplant (replacement of diseased marrow).
Marrow donors are usually relatives (siblings) or volunteers with a suitable marrow. During a bone marrow transplant, high-dose chemotherapy drugs are used to destroy the blood-forming cells in the bone marrow, then blood-forming stem cells from a matched donor are infused into the body. patient. These stem cells will develop into new, healthy blood cells to replace diseased cells.
International General Hospital Being the first and only hospital in Vietnam to successfully deploy robotic surgery. CT scans accurately detect cancer early even when there are no symptoms. Applying advanced genetic technologies for early detection of the risk of many of the most common cancers. Deploying autologous immunotherapy and thermotherapy in combination with cancer treatment to effectively prevent recurrence.
In addition, Vinmec also converges a team of leading domestic and international doctors, all of whom are highly qualified, experienced, conscientious and knowledgeable, having worked in major hospitals in Vietnam. , Korea, Russia; intensively trained at home and abroad to bring the most effective and new treatment regimens to patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
MORE
Chronic myelogenous leukemia (CML): Risk factors, stages Leukocyte defense mechanisms Risk factors for chronic lymphocytic leukemia (CLL) )