This is an automatically translated article.
The article was written by MSc Mai Vien Phuong - Gastroenterologist, Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Currently, the treatment of inflammatory bowel disease is still challenging, the diagnostic guidelines are updated regularly, requiring patient compliance, because this is a chronic, relapsing disease.
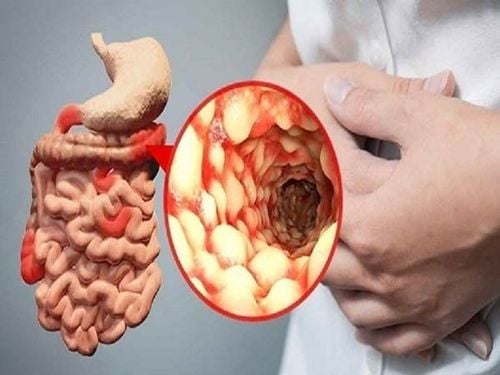
3. Diagnostic imaging in the diagnosis of inflammatory bowel disease
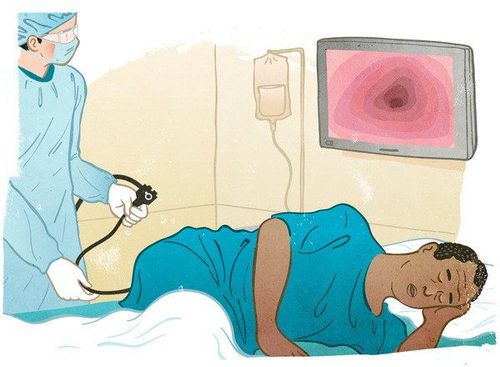
Abdominal ultrasound: Can see signs of peri-intestinal fibrosis, concentric thickening of intestinal wall, vascular proliferation CT Scan tomography of small intestine with pictures: Thickening of intestinal wall, layer by layer, concentricity, signs comb sign, intestinal stenosis Small intestine MRI : Provides very high contrast of soft tissue, both in static and dynamic images, avoids ionizing radiation Fecal calprotectin test : This is a protein secreted by neutrophils, the concentration correlates with the degree of colitis, this is a non-invasive test with advantages, limiting colonoscopy. Colonoscopy: Most valuable in diagnosing inflammatory diseases bowel, direct imaging with suggestive signs, tissue sampling for biopsies... 3.1 Differentiating inflammatory bowel disease from other inflammatory bowel diseases Differential diagnosis of inflammatory bowel disease is challenging indeed. big. Difficulties in differential diagnosis of enteritis from infectious colitis:
Enteritis can be acute in onset Stool culture may be negative in some cases of infectious colitis (due to improper sampling technique). , not enough tests, viral infection, antibiotic use...) Endoscopic images are not specific for diagnosis Histopathology also cannot be completely accurate or due to misreading of lesions (early stage) Even gastroenterologists are sometimes inexperienced in diagnosing Infections that can trigger acute exacerbations of enteritis, especially those caused by C. difficile and CMV. Clearly ( antibiotics , corticosteroids ) can falsify symptoms If symptoms subside with antibiotic use/ or think the cause is due to spontaneous remission and no recurrence of infection Most enteritis recurs in the course of of the disease, but many cases occur only at one stage
>> See more: Inflammatory bowel disease and intestinal bacteria spectrum - Article by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
4. Treatment of inflammatory bowel disease
To optimize treatment, it is necessary to treat early, treat according to risk stratification, aim for clinical remission and endoscopic remission, and monitor the treatment process with biomarkers. Measurement of drug levels is an effective tool to help explain non-response cases and guide management.
Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel diseases. These include:
Sulfasalazine (Azulfidine). Sulfasalazine can be effective in relieving symptoms of ulcerative colitis, but it has some side effects, including nausea, vomiting, heartburn, diarrhea, and headaches. Do not take this medicine if you are allergic to sulfa drugs. Mesalamine (Tidocol, Rowasa, others), balsalazide (Colazal), and olsalazine (Dipentum). These drugs often have more side effects than sulfasalazine. Take them in tablet form or use them rectally, in an enema or suppository form, depending on the area of the colon affected by ulcerative colitis. Your doctor may prescribe a combination of two different forms, such as an enema and or suppository. Mesalamine can reduce signs and symptoms in more than 90 percent of people with mild ulcerative colitis. Corticosteroids. Corticosteroids can help reduce inflammation, but they have numerous side effects, including weight gain, excessive facial hair, high blood pressure, type 2 diabetes, osteoporosis, and increased susceptibility to infections. Doctors usually only use corticosteroids if you have moderate to severe inflammatory bowel disease that has not responded to other treatment. Corticosteroids are not for long-term use and are usually prescribed for a period of 3 - 4 months.
Can also be used in combination with other drugs as a means to induce remission. For example, corticosteroids can be used with suppression of the immune system - corticosteroids can induce remission, while the immune system can help maintain remission. Occasionally, your doctor may also prescribe short-term steroid enemas to treat disease in the colon or rectum.
4.1 Suppresses the immune system These drugs also reduce inflammation, but the goal is the immune system rather than the intrinsic treatment of inflammation. Because immunosuppression can be effective in treating ulcerative colitis, scientists theorize the damage to digestive tissues is caused by the body's immune response to an invading virus or bacteria. even by itself. By this inhibitory response, inflammation is also reduced. Immunosuppressants include: Azathioprine (Azasan, Imuran) and mercapxopurine (Purinethol). Because azathioprine and mercapxopurine work slowly - three months or so to start working, sometimes combined with corticosteroids at first, but the latter seems to produce its own benefits. Side effects may include allergic reactions, bone marrow failure, infection, hepatitis, and pancreatitis. There is also some risk of developing cancer with these drugs. If you're taking one of these medications, you'll need to follow up closely with your doctor and have your blood checked regularly to look for side effects. If you already have cancer, discuss it with your doctor before starting these medications.

Cyclosporine (Gengraf, Neoral, Sandimmune). This medicine is usually for people who have not responded well to other medications or who are facing surgery due to severe ulcers. In some cases, cyclosporin can be used to delay surgery until well enough to undergo the procedure, in others it is used to control signs and symptoms until they are well enough to undergo the procedure. Other drugs start to work. Cyclosporine starts working in 1-2 weeks, but because it has the potential for serious side effects, including kidney damage and fatal infection, talk to your doctor about the risks and benefits. benefit of treatment. There is also some risk of cancer with these drugs, so let your doctor know if you have ever had cancer. Infliximab (Remicade). This medicine is specifically for people with moderate to severe ulcerative colitis who have not responded to or cannot tolerate other treatment. It works by disabling a protein produced by the immune system known as tumor necrosis factor (TNF). Infliximab recognizes TNF in the blood and removes it before it causes intestinal inflammation. Some people with heart failure, people with multiple sclerosis, and people with cancer or a history of cancer cannot take infliximab. The drug is associated with an increased risk of infections, especially tuberculosis, and triggers viral hepatitis, which may increase the risk of blood problems and cancer. A skin test for tuberculosis is required before infliximab is administered.
Additionally, because it contains the rat infliximab protein, it may cause serious allergic reactions in some people - reactions that may be delayed from days to weeks after starting treatment. When started, infliximab is usually continued as long-term treatment.
4.2 Nicotine Patches Skin patches — the same ones used to quit smoking — seem to provide short-term relief for mild ulcerative colitis for some people. It's unclear exactly how the nicotine patch works, and the evidence it provides better effects than other treatments is disputed among researchers.
Patients should talk to their doctor before attempting treatment. One thing is clear, however, that the overall health risks from smoking far outweigh any potential benefits that nicotine may provide, so don't start smoking to treat ulcerative colitis. colon.
4.3 Other medications In addition, to control inflammation, certain medications can help relieve signs and symptoms. Depending on the severity of your ulcerative colitis, your doctor may recommend one or more of the following:
Antibiotics. People with febrile ulcerative colitis will likely be given antibiotics to help prevent or control infection. Anti-diarrheal. Fiber supplements such as psyllium powder (Metamucil) or methylcellulose (Citrucel) may help reduce the signs and symptoms of mild to moderate diarrhea. For more severe diarrhea, loperamide (Imodium) may be effective. However, use antidiarrheal drugs, with caution, because they increase the risk of megacolon. Iron supplement. If there is chronic intestinal bleeding, it is possible to develop iron-deficiency anemia. Iron supplementation can help restore normal iron levels and reduce anemia.

4.4 Surgery If diet and lifestyle changes, medication, or other treatments don't relieve your signs and symptoms, your doctor may recommend surgery.
Surgery can often remove ulcerative colitis. But that usually means removing the entire colon and rectum (proctocolectomy). After this surgery, a small bag will be worn through a hole in the abdomen (ileostomy) to collect stool.
However, a procedure called ileoanal eliminates the need to carry a bag. Instead, the surgeon creates a pouch from the end of the small intestine. This holster is then attached directly to the anus. This allows for the expulsion of more waste than usual, although there may be more bowel movements, frequent discharge or watery discharge because there is no colon to absorb water.
If having surgery, ask your doctor about ileostomy or ileoanal as appropriate. Between 25 and 40 percent of people with ulcerative colitis eventually need surgery.
4.5 Pregnancy Women with ulcerative colitis can often have a successful pregnancy, especially if they can keep the disease in remission during pregnancy. There is a slight increased risk of preterm birth and low birth weight infants. Ideally, you will get pregnant when the disease is in remission.
Some medications may not be indicated for use during pregnancy, especially during the first trimester, and the effects of some medications may linger after stopping them.
Talk to your doctor about the best way to manage the disease before conception. If certain medications are stopped, their effects may be prolonged. It is estimated that the risk of ulcerative colitis passed on to the offspring if the partner does not have ulcerative colitis is less than 5 percent.
At Vinmec Hospital, the diagnosis through colonoscopy with Olympus CV 190 endoscope, with NBI function (Narrow Banding Imaging - endoscopy with narrow light frequency band) gives analytical image results. mucosal pathology is more obvious than conventional colonoscopy, detecting ulcerative lesions in the colon.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.