This is an automatically translated article.
The article was written by MSc Mai Vien Phuong - Gastroenterologist, Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Inflammatory bowel disease (IBD) is a chronic inflammatory bowel disease that results from an excessive and prolonged immune response in the gastrointestinal mucosa to a certain antigen (food/bacteria). ...) on a particularly susceptible genetic basis, this is a disease with a period of remission and recurrence, which can "last a lifetime", the cause and "pathogenesis" are unknown but related. to immunity.
1. Diseases of inflammatory bowel disease
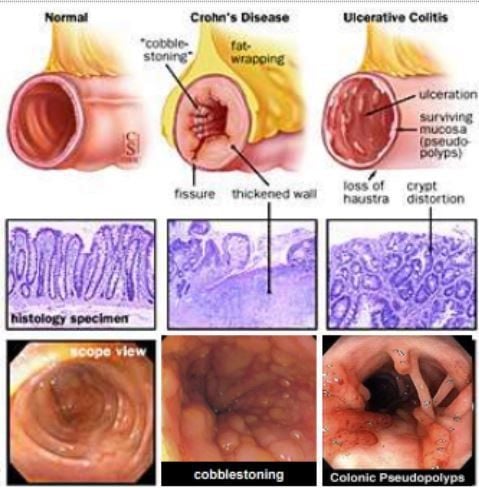
Two forms of inflammatory bowel disease:Ulcerative Colitis (UC): Ulcerative colitis (hemorrhagic); Crohn's disease (CD): Crohn's disease, in addition may have an indeterminate form.
1.1 Crohn's Disease Crohn's disease is a complex of chronic diseases that primarily affect the digestive system. This disease involves an abnormal immune response that causes excessive inflammation. It usually affects the walls of the intestine, especially the lower part of the small intestine (ileum) and segments of the colon.
However, inflammation can affect any part of the digestive tract, from the mouth to the anus. Inflammatory segments become thickened and edematous and on the inner surfaces may develop ulcers. It causes inflammation of the digestive tract, leading to abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition.
Inflammation in Crohn's disease can affect many different areas of the gastrointestinal tract, for different ethnicities. Inflammation in Crohn's disease often extends down to the layers of the inflamed intestinal wall. Crohn's disease is both painful and debilitating and can sometimes cause life-threatening complications. Although no definitive treatment is known, treatments can reduce many signs and symptoms, including long-term remission. With treatment, many people with Crohn's disease can still lead a good life.
1.1.1 Gastrointestinal symptoms In some patients, only the last part of the small intestine (the ileum) is affected. In others, the disease is localized to the colon. The most commonly affected areas are the terminal small intestine and colon.
Signs and symptoms of Crohn's disease can range from mild to severe. They usually develop slowly, but can sometimes turn severe without warning. You may also have periods without symptoms (remission). When the disease is active, signs and symptoms include:
Diarrhea Fever Fatigue Abdominal pain, cramping Blood in stools Pain in the mouth Loss of appetite and weight loss Pain or leakage near or around the anus due to percutaneous fistula Confirm disease by contrast enterography or endoscopic ± biopsy.
1.1.2 Causes The exact cause of Crohn's disease is unknown. It was previously thought to be due to diet and stress, but now doctors know that these factors can make the disease worse, not cause Crohn's disease. A number of factors such as genetics and a weak immune system may play a role in the development of the disease.
Immune system. It is possible that a virus or bacteria causes Crohn's disease. As the immune system tries to destroy invading bacteria, an abnormal immune response can also cause the immune system to attack the cells of the digestive tract. Genetic. Crohn's disease is more common in a family member with the disease, so genes may play a role in making people more susceptible to the disease. Up to 15% of people affected are first-degree relatives (parents, siblings, children) but in general the majority of people with Crohn's disease have no family history of the disease. 1.1.3 Risk factors for Crohn's disease Age. Crohn's disease can occur at any age but is most common when you are young. Most are diagnosed around the age of 30. It is common in late teens or early 20s, although the disease can begin at any age. Tends to be repeated many times in life. In some cases, inflammation of the joints, eyes, or skin also occurs. Race. Although Crohn's disease can affect all races, it is more common in Western Europe and North America (100-300 people/100,000 population); More than half a million Americans are currently suffering from this disease. The most common are Nordic and Central European Jews. However, the incidence is now increasing among blacks living in North America and the UK. Genetic variations, environment and life factors. It is said that the cause is a combination of these three types of factors. Most are related to the NOD2, ATG16L1, IL23R and IRGM genes that influence immune system function. There are at least 200 genetic variations that increase the risk of Crohn's disease. Family history. You are at higher risk when you have a first-degree relative with the disease. Smoke. This is the most important factor that can be controlled. Smoking also makes the disease worse and increases the risk of surgery. If you are a smoker, the most important thing is to stop smoking.
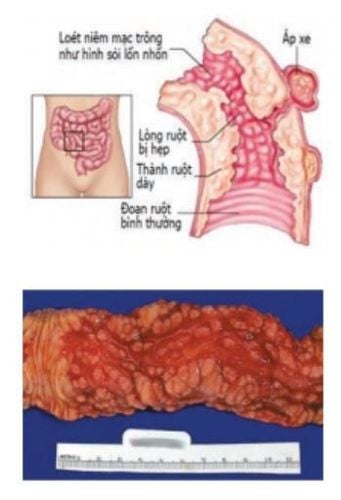
Non-steroidal anti-inflammatory drugs. These include: ibuprofen (Advil, Motrin IB...), naproxen sodium (Aleve), diclofenac sodium (Voltaren) and others. While they do not cause Crohn's disease, they can cause intestinal inflammation that makes Crohn's disease worse. Where do you live. If you live in an urban or industrialized country, you may be more susceptible to Crohn's disease. This suggests that environmental factors, including a diet high in fat or refined foods, may play a role in Crohn's disease. 1.1.4 Crohn's disease resulting in one or more complications of Intestinal Obstruction. Crohn's disease affects the thickness of the intestine. Over time, portions of the intestine can become severely swollen or scarred and narrow, which can impede the flow of food through the digestive tract. You may need surgery to remove this pathological segment of bowel. Ulcers . Chronic inflammation can lead to ulcers elsewhere in the gastrointestinal tract, including the mouth and anus, and in the genital tract (perineum). Leaks . Sometimes ulcers can penetrate the entire thickness of the intestinal wall, creating fistulas, which can open to the skin or communicate with another organ. Fistulas near or around the anus are the most common type. As fistulas develop in the abdomen, food can pass through the intestinal passages, reducing absorption. Fistulas may occur between loops of bowel, into the bladder or vagina, or may open to the skin, causing a persistent fistula of bowel contents. In some cases, the fistula becomes infected and creates an abscess that can be life-threatening if left untreated. Anal fissure. This is a small tear in the tissue lining the anal canal or the skin around the anus, which is very susceptible to infection. It is often associated with painful bowel movements and can lead to perianal fistulas. Poor nutrition. Diarrhea, abdominal pain, and cramping can make it difficult for you to eat or for your intestines to absorb nutrients. You are more likely to develop anemia due to a lack of iron and vitamin B12 caused by the disease. Colon cancer . Crohn's disease increases the risk of colon cancer. General colon cancer screening guidelines for people without Crohn's disease require a colonoscopy every 10 years beginning at age 50. Ask your doctor if you should have this screening earlier and more often. or not.

Other health problems. Crohn's disease can cause other problems in other parts of the body. Among these problems are anemia, skin disorders, osteoporosis, arthritis and diseases of the bladder or liver. Medical risks. Some medications for Crohn's disease work by suppressing immune system functions with a small risk of developing diseases such as malignant tumors of the lymphatic system and skin cancers. They also increase the risk of bacterial infection. Corticosteroids can increase the risk of osteoporosis, fractures, cataracts, glaucoma, diabetes and high blood pressure... Talk to your doctor to determine the risks and benefits of these medications. curative drugs. 1.1.5 Nutrition in the treatment of Crohn's disease Diet: Eliminate: processed milk, sugar, gluten (a substance found in wheat and cereal grains), alcohol, coffee, processed foods. Replace with: fresh fruits, vegetables, clean fats and proteins; Monitor symptoms: eliminate the inappropriate Drink plenty of fluids: water, herbal teas, kombucha drinks Manage stress: yoga, exercise, contemplation... Supplements: natural supplements in vitamins, essential minerals, vitamin B12, iron... Avoid drugs: antibiotics, birth control pills, NSAIDs... Supplement the gut with good bacteria: probiotics .. 1.2 Ulcerative colitis This is also one of the two main types of inflammatory bowel disease, characterized by chronic inflammation of the gastrointestinal tract. There are similarities between ulcerative colitis and Crohn's disease, but also differences.
Similarities:
Both are teenagers and adults in their 20s and 30s, but can get the disease at any age. Both have the same ratio of men and women. The symptoms are very similar. The cause of the two diseases is unknown because both diseases have similar types including constitutive factors such as environment, genetics and inappropriate response to the body's immune system.
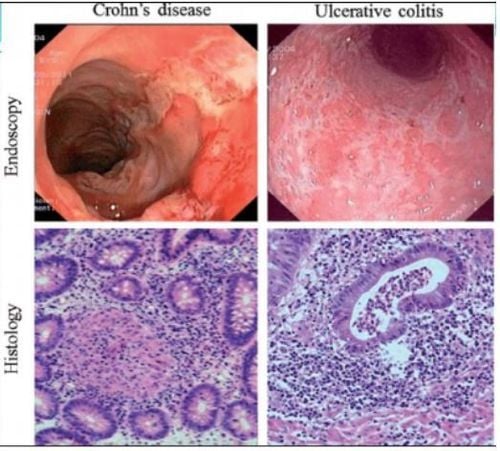
1.2.1 Differences between the two diseases Crohn's disease can be found in many places throughout the digestive tract from the mouth to the anus, most commonly in the terminal small intestine (ileum); Unlike in ulcerative colitis, the inflammation is only localized to the colon-rectum. In Crohn's disease, inflammatory segments alternate with benign segments and may appear in patches; Unlike in ulcerative colitis, inflammation is continuous throughout a long segment of the colon. In Crohn's disease, lesions can occur in all layers of the intestinal wall, can penetrate the entire thickness of the intestinal wall, so there is a risk of narrowing the gastrointestinal tract later; Unlike in ulcerative colitis, which involves only the innermost layer of the colon (mucosa), there is no risk of bowel obstruction. Crohn's disease often causes fistulae into adjacent organs: bladder, uterus, anal fistula, whereas ulcerative colitis does not present a risk of fistula. Crohn's disease

1.2.2 Risk factors for ulcerative colitis Age. Ulcers can occur at any age, but usually affect people in their 30s. Some people may not develop symptoms until age 50 or 60. Race or ethnicity. Caucasians are at the highest risk of the disease. If you are of Jewish descent, the risk is even higher. Family history. There is a high risk if you have a close relative, such as a brother, parent or child, with the disease. Use isotretinoin (Accutane). Isotretinoin (Accutane) is a medication that is sometimes used to treat acne scars that are cystic or have not responded to other treatment. Although causality has not been proven, studies have reported the development of inflammatory bowel disease with isotretinoin use. Non-steroidal anti-inflammatory drugs. Although these drugs - ibuprofen (Advil, Motrin, others), naproxen (Aleve), diclofenac (Cataflam, Voltaren), piroxicam (Feldene and others) - have not been confirmed to cause ulcerative colitis, can cause similar signs and symptoms. In addition, these drugs can make existing ulcerative colitis worse, and may make the initial diagnosis more difficult. About 10% of inflammatory bowel diseases have features that are typical of both diseases, namely colitis indeterminate.
At Vinmec Hospital, the diagnosis through colonoscopy with Olympus CV 190 endoscope, with NBI function (Narrow Banding Imaging - endoscopy with narrow light frequency band) gives analytical image results. mucosal pathology is more obvious than conventional colonoscopy, detecting ulcerative lesions in the colon.
>> See more: Inflammatory bowel disease and intestinal bacteria spectrum - Article by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.