This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Bui Thi Ha - Pediatrician - Neonatologist - Department of Pediatrics - Neonatology - Vinmec Ha Long International General Hospital.1. What is neonatal jaundice?
Neonatal jaundice due to indirect hyperbilirubinemia is common. In neonates, indirect hyperbilirubinemia may occur in 60% of term infants and 80% of preterm infants. The disease can be mild (physiological jaundice) or severe (pathological jaundice). The disease needs to be detected early and treated promptly to avoid serious complications, which can result in death or lifelong cerebral palsy.2. Causes of pathological neonatal jaundice
Jaundice occurs early from day 1 to 2 after birth: Mainly due to hemolytic causes, rare. Common causes are maternal and child blood group incompatibility, immune hemolysis, G6PD deficiency. Jaundice occurs when the mother has Rh factor (-) and the baby is born with Rh factor (+). When the mother is pregnant, some of the Rh (+) fetus's red blood cells enter the Rh (-) mother's blood. The mother's body responds by producing anti-Rh (+) antibodies. These antibodies enter the body of the fetus, causing hemolysis. In addition to jaundice, the child also had anemia, bleeding, enlarged liver and spleen.Jaundice occurs from 3 to 10 days postpartum: Usually due to umbilical cord infection, skin infection, sepsis; Polycythemia vera, hemangioma, serous tumor; slow digestion of meconium, intestinal atrophy;
Jaundice lasting more than 14 days: Mainly due to breast milk, infants with liver disease, biliary obstruction, congenital hypothyroidism or metabolic disease.

3. Sequelae of jaundice due to increased indirect Bilirubin
Transient Encephalopathy: A condition in which a pediatric patient is poisoned by an early, transient increase in bilirubin. Clinical manifestations are lethargy, lethargic children. Nuclear jaundice: An encephalopathy caused by untreated hyperbilirubinemia, the progression of permanent nerve damage is nuclear jaundice. Manifestations through 3 stages: Stage 1: Appears in the first days, the child is somnolent, has decreased muscle tone, sucks poorly, cries; Stage 2: Appears immediately after birth or in the first week after birth, the baby refuses to breastfeed, increases muscle tone, fever, convulsions, convulsions, or flexes the neck and body, possibly death in apnea. Stage 3: Occurs 1 week after birth, with sequelae, hypertonia, coma, convulsions, visual and hearing abnormalities.4. Change of blood in neonates with jaundice
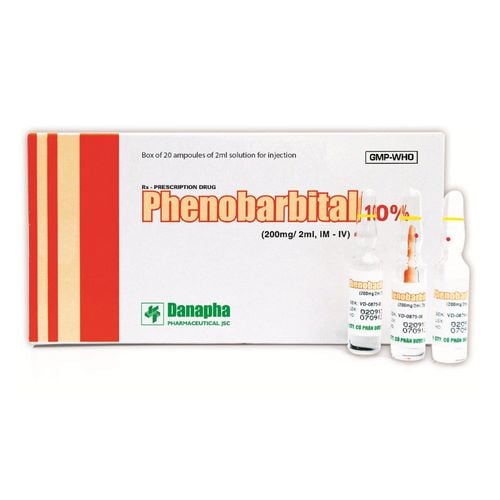
A blood transfusion is a procedure in which a portion of hemolytic erythrocytes with antibodies and immature antibodies are removed in co-immune hemolytic disease, resulting in increased free bilirubin in the blood, and replaced with donor blood. Exchange transfusion is also used in other cases when the bilirubin in the blood is too high to be neurotoxic.4.1. Note when changing blood Should check Bilirubin levels in the blood in children: Jaundice from the first day after birth; jaundice appearing from day 2 in premature infants less than 35 weeks; jaundice to palms and soles at any age; Neonates should be irradiated before a blood transfusion is indicated; Assessment of acute brain complications due to increased free bilirubin in the blood; 4.2. Indications for blood transfusion Clinical: Generalized dark yellow skin (less than 1 week), neurological abnormalities begin Or high blood indirect bilirubin level > 20mg%, neurological abnormalities such as lethargy, poor feeding. 4.3. Contraindications for blood exchange Hemodynamic instability; Severe respiratory failure or shock; The umbilical catheter cannot be placed; No suitable blood and fresh blood (less than 5 days). In the case of not being able to exchange blood, an alternative treatment can be applied, which is continuous double-sided light and possibly additional infusion of Albumin, Phenobacbitan

Complications related to umbilical vein catheters; Infection from a blood bag or procedure; Hyperthermia or hypothermia Anemia, thrombocytopenia Electrolyte disturbances, acid-base, blood sugar; Necrotizing enterocolitis Hemolysis due to forceful pumping or withdrawing. Blood exchange is the technique indicated for the treatment of severe jaundice in neonates when the disease is at risk of causing neurotoxicity. When giving your baby this treatment, it is necessary to strictly follow the instructions of the doctor to ensure the highest treatment effectiveness and avoid possible sequelae.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.