This is an automatically translated article.
Articles by Master, Doctor Tran Quynh Trang - Doctor of Biochemistry - Laboratory Department - Vinmec Times City International Hospital
Copper is an indispensable substance in the human body, ceruloplasmin is a protein that contains copper, participating in the body's copper metabolism. In the liver, copper binds to ceruloplasmin to form ceruloplasmin which then releases it into the bloodstream. To diagnose Wilson's disease or evaluate copper metabolism, your doctor will order a ceruloplasmin test.
1. What is Wilson's disease?
Wilson's disease is a relatively rare disease. This is an autosomal recessive allele disorder caused by mutations in the ATP7B gene, resulting in the deficient production of the copper transporter adenosine triphosphatase 2 (ATPase2). This protein has a dual role in copper homeostasis. Its function is to transfer copper to the Golgi apparatus to supply it to copper transport proteins. Its function changes in the presence of excessive intracellular copper levels. ATP7B alters its intracellular location with respect to the apical membrane of hepatocytes to promote copper excretion into bile. As a result, defects in the hepatic excretory pathway lead to impaired copper excretion into the bile leading to copper accumulation.
2. Symptoms of Wilson's disease
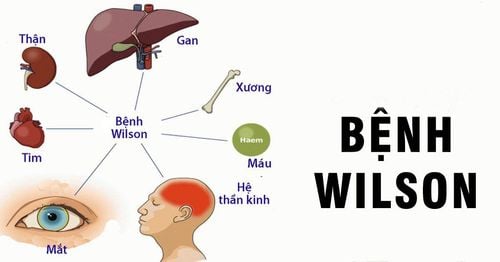
Symptoms of Wilson's disease can be hepatic, neurological or psychiatric. Diagnosis is test-based, and the availability of genetic tests in conjunction with clinical symptoms makes the diagnosis more accurate, especially in heterozygous patients or those with blocked bile.
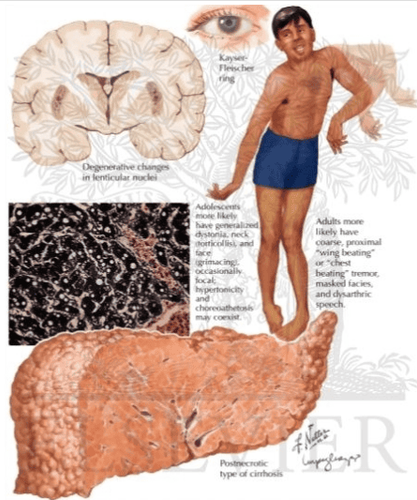
Neurological symptoms usually appear later than liver symptoms. Initial liver symptoms occur in nearly 40% of patients, neurological symptoms in 40%-50% and psychiatric symptoms in 10% of patients. Approximately 10% of patients are asymptomatic when diagnosed with Wilson's disease, which is usually diagnosed during examination of a sibling of the affected group or during routine testing for elevated liver enzymes. clear cause. Hepatic symptoms range from mild to severe, which can range from asymptomatic to life-threatening liver failure, with approximately 5% of patients rapidly progressing to fulminant Wilson's disease despite previously being otherwise healthy. Most patients with liver symptoms have signs of chronic liver disease with cirrhosis, portal hypertension, and Coombs-negative hemolytic anemia, which can lead to acute renal failure. in critically ill patients. Transient hemolytic jaundice may be the initial symptom in patients without any other signs of liver disease.
The initial neurological symptoms are subtle, difficult to detect and nonspecific, difficult to exploit due to difficulties in concentration, lack of coordination, altered spelling and slurred speech accompanied by drooling. Some obvious neurological symptoms such as: arrhythmia, dystonia, tremor and parkinsonism. Tremor is one of the most common neurological signs in 22-55% of patients diagnosed with Wilson's disease. Tremor occurs when the patient straightens the arm, the amplitude of the tremor increases with longer holding time, and many patients present with a violent pulsating tremor with a large amplitude.

Dystonicity is another common neurological manifestation of Wilson's disease and is present in 10% to 65% of patients. It is characterized by abnormal posture of various body parts often associated with twitching or twisting movements. It may be focal, such as forceful eye closure due to cerebral spasm, such as involuntary head rotation associated with unilateral shoulder elevation as seen in spasmodic myoclonus. Segmental or focal craniocerebral dystonia particularly symptomatic with severe dyspnea, cardiac arrhythmias, dystonia with forced, frequently exaggerated smiles and dysphagia with complete loss of speech and inability to swallow. Severe Wilson's disease can lead to systemic dystonia, leading to abnormal posture of the trunk, neck, or extremities and subsequently to debilitating symptoms with secondary skeletal changes and inability to can walk. Less common neurological problems include spasticity, chorea, neurosis, or myoclonus.
Overall, about half of patients with Wilson's disease have neuropsychiatric symptoms. Frank's psychosis is present in about 10% of these patients and is often misdiagnosed as schizophrenia or bipolar. Behavioral and personality changes often include lack of concentration, compulsive or impulsive behavior, and apathy. Eye damage is also a possible symptom but difficult to detect. Accumulation of copper causes copper deposition in the cornea forming a Keyer-Fleischer ring, copper deposition in the retina and vitreous causing a sunflower cataract.
Wilson's disease is an autosomal recessive genetic disease that usually affects males and females equally, but has important sex-specific phenotypic differences. Liver symptoms are more common in women, accounting for 55%–60% of all cases with liver symptoms. Women also tend to have the onset of symptoms about 2 years later than men.
Other systemic manifestations of Wilson's disease are rare and difficult to recognize. Age of onset varies widely from 5 to 35 years with variable and nonspecific clinical manifestations. Late diagnosis can lead to worsening of liver and neurological symptoms. As the delay in diagnosis increases from 1 to 6 months, only about one-fifth of the patients achieve a favorable outcome with very mild disability. However, the median time from symptom onset to accurate diagnosis and appropriate treatment remains unsatisfactory with a median time of ~1 year from onset to diagnosis. This is one of the reasons why many patients experience irreversible neurological problems or structural changes in the liver.
3. Diagnosis of Wilson's disease
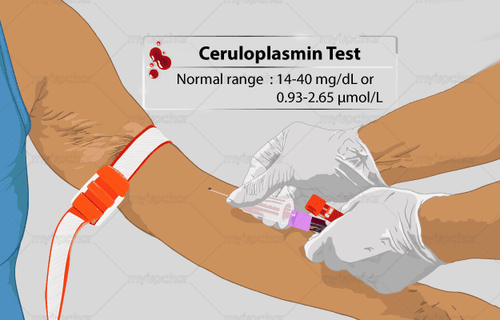
Ceruloplasmin test
Plasma ceruloplasmin concentration is recommended as the first step in the diagnosis of Wilson's disease and as a screening laboratory test. Serum ceruloplasmin levels <20 mg/dL (200 mg/L or 2.83 μmol/L) are diagnostic but overall the positive predictive value is very low at 5.9%. Ceruloplasmin is a copper-binding plasma protein. Up to 95% of copper in the blood is bound to ceruloplasmin.
Normal value of ceruloplasmin: 20 – 60 mg/dL. This value may vary by room and test method.
Cerulopasmin increases in case the patient is pregnant, taking birth control pills... Ceruloplasmin decreases in case the patient has Wilson's disease, Menkes disease. Copper testing
Every patient with suspected Wilson disease should have a 24-hour urine copper test, and this test alone is diagnostic in many patients. It is important to completely collect urine for 24 hours beginning after the first morning urinating on the day of collection and completing the following day, emptying once at the end. Another specification is that the collection vessel does not contain copper. A 24-hour copper value > 100 μg/24 h (1.6 μmol/24 h) is generally considered diagnostic of Wilson's disease. This is certainly true for patients with neurological or psychiatric manifestations. However, in patients with chronic cholestasis or autoimmune hepatitis may also have values >100 μg/24 h, additional testing is needed to distinguish this from Wilson's disease.
Liver copper testing is considered the gold standard to confirm the diagnosis and may be ordered in patients with predominantly hepatic manifestations. However, a diagnosis of neurological or psychiatric Wilson's disease is sufficient based on diagnostic values of 24-hour urinary copper excretion.
The plasma copper test is also one of the factors that help diagnose Wilson's disease. Total serum copper includes co-bound and free (unbound) copper. The total copper value alone is not very helpful in diagnosing Wilson's disease because it is highly variable and often parallels the major copper-binding protein ceruloplasmin. Most laboratories consider the range 65–140 μg/dL (10–22 μmol/L) to be normal.
MRI
Structural and functional imaging can to some extent be helpful in diagnosing Wilson's disease. Magnetic resonance imaging (MRI) detects brain abnormalities in all patients with essentially neurological symptoms. However, these changes are not specific and Wilson's disease needs to be confirmed by other methods.
Untreated Wilson's disease will inevitably lead to liver, neurological or mental problems, or various combinations of them. The goals of treatment in Wilson's disease are to reverse copper overload and establish a copper balance in which copper values are reduced to normal. The second step is to maintain these levels without causing harmful copper shortages. Maintenance therapy is initiated after disease symptoms and biochemical abnormalities have improved, and this is usually observed for 2–6 months after initiation of chelation therapy. Unless the patient undergoes a liver transplant, the maintenance phase is a lifelong therapy.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Bull PC, Thomas GR, Rommens JM, Forbes JR, Cox DW. The Wilson disease gene is a putative copper transport P-type ATPase similar to the Menkes gene. Tanzi RE, Petrukhin K, Chernov I, et al. The Wilson disease gene is a copper transport ATPase with homology to the Menkes disease gene. Brewer GJ. Wilson's Disease: A Clinician's Guide to Recognition, Diagnosis, and Management. Norwel, MA: Kluwer Academic Publishers; 2001.