This is an automatically translated article.
Scleroderma is one of the autoimmune diseases, when the immune system does not perform its protective function, but instead attacks healthy cells. Doctors currently do not know the cause of scleroderma, as well as how to prevent scleroderma effectively.
1. What is scleroderma?
Scleroderma is a chronic disease that affects the skin, connective tissue and internal organs. It occurs when the immune system malfunctions, causing the body to make too much of the protein collagen, an important part of the skin.
As a result, the patient's skin becomes thick and hard, sometimes the lungs and kidneys can form scars. Your blood vessels also thicken and don't work properly, leading to tissue damage and high blood pressure.
Scleroderma is not contagious, which means you can't get it from other people. Although there is no cure, treatment can relieve symptoms and help patients feel better.
Without proper treatment, people with autoimmune scleroderma are at risk of experiencing the following complications:
High blood pressure in the lungs; Scar tissue in the lungs; Anemia to the fingers and toes; Myositis ; Infection; CKD .

Bệnh tự miễn xơ cứng bì có nguy cơ suy thận ở người bệnh
2. Types of scleroderma
There are two types of autoimmune scleroderma:
2.1. Localized scleroderma Mainly affects the skin, occurs in 1 of 2 forms:
Localized: The skin appears hard, oval, red or purple borders, the center part turns white. . Occasionally, focal scleroderma also affects blood vessels or internal organs (generalized morphea); Banding: Causes thick lines or streaks of skin on the patient's arms, legs, or face. 2.2. Systemic scleroderma Also known as systemic scleroderma, it affects many body parts. This systemic sclerosis is further divided into 2 subtypes:
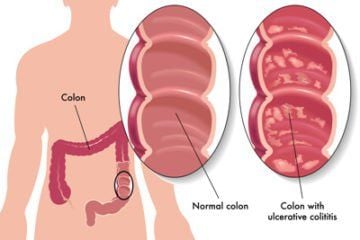
Limited sclerosis: Symptoms appear gradually and affect the skin of the face, hands, and feet. The disease can also damage the patient's lungs, intestines, or esophagus. This condition is sometimes referred to as CREST syndrome, with 5 common signs (Calcification - Raynaud's phenomenon - Esophageal dysfunction - Calluses of extremities - Varicose veins); Diffuse scleroderma: The disease progresses rapidly, with the skin in the midsection, thighs, arms, hands, and feet growing thick. The condition also affects internal organs, such as the heart, lungs, kidneys, and digestive tract.

Vùng da bị tổn thương có xu hướng dày lên
3. Causes of scleroderma
So far, doctors have not found the cause of scleroderma, so there is no effective way to prevent scleroderma. This is one of the autoimmune diseases, which occurs when the immune system, which is supposed to protect the body from germs, causes inflammation of the skin and damage to other organs.
It can be confirmed that scleroderma is not an infectious disease, nor is it passed on from parents to children. The cause of scleroderma is likely due to a combination of factors, such as:
Abnormal activity of the immune system: The patient's immune system stimulates immature fibroblasts to produce too much glue agent. These substances are deposited around cells, blood vessels and organs. Gradually causing damage and fibrosis at the deposition site; Gene structure: Several susceptibility genes contribute to the risk of onset and progression of scleroderma; Environmental hormones: Long-term exposure to certain elements in the environment, such as viruses (Borrelia infection), chemical colloids, or organic solvents, can also be a cause. scleroderma patients ; Endocrine factors: Between the ages of 30 and 55, the proportion of female patients is 7-12 times higher than that of men. For this reason, the role of female sex hormones is also discussed, especially estrogen. Autoantibodies: Common in autoimmune scleroderma are antinuclear antibodies, anti-Scl-70 antibodies and anti-centromere antibodies.
Anyone can get scleroderma, but it's most common in women between the ages of 35 and 55. Other factors that contribute to an increased risk include:
Certain changes in genome; Family history of autoimmune disease; Environmental triggers, such as viruses, drugs or chemicals.

Cấu trúc bộ GEN bị thay đổi có thể là nguyên nhân gây ra bệnh
4. Scleroderma symptoms
The symptoms of the autoimmune disease scleroderma can affect many parts of the body, including:
Hard or thick, tight, shiny skin, appearing most commonly on the hands and face; Raynaud's phenomenon; Ulcers or sores on the fingertips; Small red spots on the face and chest; Hard, oval patches on the skin; Difficulty swallowing; Joint pain or swelling; Muscle weakness; Dry eyes or mouth (Sjogren's syndrome); Swelling, mainly of the hands and fingers; Shortness of breath; Cramps and flatulence; Heartburn; Diarrhea ; Unexplained weight loss;
5. Diagnosis and treatment of scleroderma
5.1. Diagnosis The doctor will perform a physical examination and ask about the patient's medical history. Several tests may be done, such as:
Diagnostic imaging (X-ray and CT scan); Blood tests;

Phương pháp xét nghiệm máu giúp các bác sĩ chẩn đoán tình trạng bệnh
Digestive tract test; Lung function test; Heart tests (electrocardiogram and echocardiogram) Skin biopsy.
5.2. Treatment Symptoms of autoimmune scleroderma can be controlled with:
Non-steroidal anti-inflammatory drugs (NSAIDs): Ibuprofen or aspirin to help reduce swelling and pain; Steroids and drugs that suppress the immune system: To help with muscle, joint or organ problems; Medicines that increase blood flow to the fingers; Blood pressure medication; Drugs that dilate blood vessels in the lungs, avoiding scar tissue; heartburn medicine; Antibiotic; Medications to promote bowel movements Other supportive measures include:
Exercise; Add more fiber and fluids in your diet; Skin treatment with light and laser therapy; Physical therapy ;

Vật lý trị liệu giúp hỗ trợ điều trị bệnh tự miễn xơ cứng bì
Rehabilitation; Stress control, stress management; Organ transplant if severely damaged. In general, the pathogenesis of scleroderma is still unclear, so there is no effective way to prevent scleroderma. This is a chronic condition, so sufferers need to learn to live with it. Adequate information, care planning and symptom control treatment will limit the risk of serious complications.
For detailed advice, please come directly to Vinmec health system or register online HERE.
Reference source: webmd.com