This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Crohn's disease is an inflammatory bowel disease with symptoms of abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition. The inflammation caused by Crohn's disease often spreads deep into the layers of intestinal tissue, which is both painful and debilitating, and can sometimes lead to life-threatening complications.
Although there is no cure for Crohn's disease, care and treatment can significantly reduce the signs and symptoms of the disease and even bring about long-term remission.
1. History of Crohn's Disease
In the literature, there have been reported cases of Crohn's symptoms quite early. In 1612, the first case was described as a boy who died from abdominal pain and persistent diarrhea, when autopsy revealed an ulcer in the cecum causing retraction and spread to the ileum.
Then there is a very famous case of King Louis XIII of France (1600 - 1643) who had diverse features of lower gastrointestinal tract lesions including perianal abscess, intestinal obstruction and chronic diarrhea. Then, in 1806, two authors Combe and Saunders published the first cluster of cases of Crohn's, described in quite detail with cases of narrowing and thickening of the terminal ileum.
Then there were a few more case reports from the surgeon, the pathologist noted a pathology causing chronic ileocecal inflammation, which could be misdiagnosed with malignancy. By 1932, the group of authors Crohn, Ginzburg and Oppenheimer published 14 cases of patients with localized inflammatory lesions in the ileum with features such as mass at the terminal ileum due to inflammatory lesions, and lesions. Gastrointestinal fistula, evidence of bowel obstruction, patient with exhaustion, anemia and a history of appendectomy.
Two years later, Kantor et al. reported and described in more detail some features of this pathology on gastrointestinal barium imaging such as dilatation of the upper ileum and failure of the drug to descend to the terminal ileum. Due to obstruction, the adjacent loop of bowel is abnormally deposited, and the cecum area is deformed. The authors also introduced for the first time the concept of the "string sign" to describe a narrow lesion in the terminal ileum.
2. Is Crohn's disease common in the world?
Epidemiological data on chronic inflammatory bowel disease (TBD) mainly come from studies in Western countries (Europe, Australia, USA..) while studies in the region. Asia also records a low but increasing incidence of IBD
A new review published in 2018 on the worldwide prevalence of IBD shows that in the 21st century, the prevalence in the population in countries such as Canada, Denmark, Germany, Australia, Sweden, UK, USA have increased by over 0.3% and are still trending up. According to the model, by 2025, the incidence of IBD in Canada may be up to 0.9% of the population. Results of cohort studies conducted in Asia show that the prevalence of Crohn's disease is low but increasing gradually. in recent years and unevenly across countries.
In China, the prevalence varies from region to region and is correlated with population density, while in Korea, a study of national data shows that the prevalence is relatively uniform across ethnic groups. city.
In the Asia-Pacific region, a multicenter study (ACCESS study) was conducted at 21 centers in 12 cities in 9 countries over the span of one year from 2011 to 2012 and recorded 419 schools. New cases of IBD were discovered in which Crohn's accounted for 187 cases (39.6%). The annual incidence and age-adjusted incidence rates vary from country to country, with the lowest incidence in parts of China, Thailand, and Indonesia and the highest in Australia.
According to this study, in the Asian region, the median age of Crohn's disease was 34, in which the age at most detection was between 20 and 24 years old with the median time from symptom onset to diagnosis. defined as 5 months. The disease is more common in men (61.4%). The location of lesions recorded in this study was similar between Asian countries and Australia, but the Asian group of patients showed more severe symptoms and had more complications. The proportion of patients with complications such as perforation, fistula, stricture and perianal lesions was higher in the Asian studies than in the Australian group (52% vs 24%, p=0.001).
3. Pathogenesis of Crohn's disease
The full pathogenesis of Crohn's disease is currently unknown, but interactions between the body's immune, microbiological, and genetic factors and environmental influences are thought to play an important role. Environmental factors here can be smoking, use of non-steroidal anti-inflammatory drugs (NSAIDs), foreign antigens affecting the stability of the intestinal mucosa thereby triggering a response. inflammation, bacterial invasion and consequent tissue destruction. To date, studies have identified more than 40 microorganisms including bacteria, viruses, fungi and more than 100 genes involved in the complex pathogenesis of Crohn's disease.This helps confirm more firmly the hypothesis of the interaction between environmental factors and genetic factors and changes in the body's immunity.
3.1. Environmental factors
For the average person, the process of exposure to antigens is quite diverse, especially in the early stages of life, helping to create a healthy immune system. A "lack of exposure" may play a role in the progression of Crohn's. This hypothesis is derived from studies in experimental and mouse models of colitis induced on the basis of a suitable genetic predisposition. When the lab mice were put in a completely bacteria-free environment, immediately, the colitis progressed very badly. In fact, epidemiological studies have also shown that Crohn's has a higher prevalence in urban areas where sanitation is better and exposure to pathogens is poorer.Some factors related to lifestyle and eating habits have been shown to be related to Crohn's such as smoking history, stress, depression, use of NSAIDs, aspirin, antibiotics... increased risk of disease progression while a diet rich in fiber, fruit and zinc was protective.
In recent years, more and more new approaches focus on studying the role of gut microbiota in chronic inflammatory bowel diseases. In the normal human, this microbiome consists of 1013,1014 bacterial cells and an estimated 1,000 different strains of bacteria. The strains with the highest percentage were Bacteroidetes, Firmicutes followed by Proteobacteria, Actinobacteria, Fusobacteria and Verrucomicrobia. In chronic inflammatory bowel diseases, there is a decrease in the density and diversity of the gut microbiota. Biopsy fragments from the patient showed a decrease in Firmicutes and Bacteroidetes strains as well as increased numbers of Proteobacteria and Actinobacteria strains. Some pathogenic bacteria, such as Escherichia coli, are highly concentrated in the affected areas of the ileum in Crohn's.
Besides bacteria, viruses and fungi are also thought to play a role in initiating inflammation in the gut and affecting immune function in chronic inflammatory bowel diseases.

3.2. Genetic factors
Observational studies reported that up to 35% of IBD patients had a family history of the disease, and this risk increased to 50% for identical twins, leading to the hypothesis that genetic factors play a role. . To date, more than 300 nucleotide polymorphisms have been identified in more than 100 related genes, of which about 30 sites have been identified with Crohn's involvement. Most of these genes have roles in the regulation of immune mechanisms including barrier function and phagocytosis. To date, 92 base-pair substitution polymorphisms have been identified in genes involved in the activation of immune cells and intestinal epithelial cells in IBD. Initially, the activated innate immune system will stimulate a series of inflammatory factors and also acquired immune mechanisms, thereby leading to damage to intestinal cells.. In the future, the findings are hoped. New insights into the role of genetic factors will help individualize treatment and predict patient response.
3.3. Immune factor
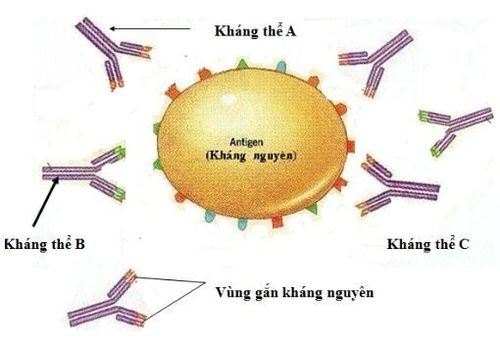
The innate immune system is initially activated by the recognition of pathogen-associated molecular patterns (PAMPs) or damage associated molecules (damage associated molecules). pattern - DAMP) is formed when cells are damaged. Once recognized by pattern recognition receptors (PRRs) located on affected cells, they lead to the production of IgA, pro-inflammatory cytokines and epithelial cell proliferation, followed by a series of responses. candidate is activated. The receptors that have been identified to participate in the pathogenesis of Crohn's include the Toll-like receptor (TLR) group, of which TLR2 and TLR4 have been studied the most. TLR2 is responsible for detecting bacterial proteins while TLR4 is capable of detecting lipopolysaccharides (LPS) in the outer coat of gram-negative bacteria. Because TLR4 has a direct effect on activating chemical mediators such as interferons and TNF-α, Crohn's patients have more TLR4 receptor expression than normal subjects, leading to a stronger inflammatory response.
In addition, another group of receptors called NOD2 or CARD15 was found to recognize the components of muramyl dipeptides in the bacterial envelope. Several studies in Europe and North America have reported that up to 50% of Crohn's patients have abnormalities in the gene that regulates the expression of NOD2 receptors.
Mechanisms of the innate immune system affected in Crohn's disease that have been identified include: Altered epithelial barrier protective function, bacterial recognition, and phagocytosis. The mucous layer on the surface of the epithelial cells has a protective effect, and the junctions between the intestinal cells help prevent bacteria from entering the intestinal lumen. The major components of the mucous layer are the glycoproteins and prostaglandin E2 which play a role in the repair of epithelial mucosal lesions. Several studies have shown that mutations of the MUC2, MUC19 and PTGER4 (prostaglandin E2 receptor 4) genes play a role in Crohn's progression [25, 26]. In addition, the production of cytokines, attracting dendritic cells and leukocytes will concentrate the bacteria on the surface of intestinal cells, thereby causing phagocytosis and antigen presentation, a step. important in the activation of the acquired immune system. Macrophages that produce proinflammatory factors activate natural killer (NK) cells that produce INFY, a chemotactic that activates dendritic cells. Next, dendritic cells produce TNE-q, which mobilizes other inflammatory cells.

Of the mechanisms of activation of the acquired immune system in Crohn's disease, the role of T cells is dominant. After antigen-presenting cells bind to antigens, these cells follow the lymphatic system back to intestinal lymphoid organizations such as mesenteric lymphoid follicles and Peyer's mucous membranes for presentation to cells. T cells and T cell differentiation will take place to form helper and regulatory T cell lines. These cells then again produce specific cytokines and play a role in the regulation of the gut microbiota as well as suppressing the immune response. In Crohn's, the cell lines identified that play an important role include Thi, Th17 and several regulators.
Vinmec Hospital with modern facilities and equipment and a team of experienced experts, always dedicated to medical examination and treatment, customers can be assured of gastroscopy and esophagogastroduodenoscopy services. at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesDao Van Long, Dao Viet Hang. Autoimmune allergic disease of the gastrointestinal tract. Medical Publisher. Bernstein C. N. and Shanahan F. (2008). Disorders of a modern lifestyle: reconciling the epidemiology of inflammatory bowel diseases. Gut,57(9), 1185 - 1191. 3. Nell S., Suerbaum S., and Josenhans C. (2010). The impact of the microbiota on the pathogenesis of IBD: lessons from mouse infection models. Nat Rev Microbiol, 8(8),564-577. 4. Binder V. (1998). Genetic epidemiology in inflammatory bowel disease. Dig Dis Basel Switz, 16(6), 351-355. 5. Montgomery S. M., Morris D. L., Pounder R. E. et al (1999). Asian ethnic origin and the risk of inflammatory bowel disease. Eur J Gastroenterol Hepatol, 11(5),543-546. 6. Frank D. N., St Amand A. L., Feldman R. A. et al (2007). Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA, 104(34), 13780-13785. 7. OttS, J., Musfeldt M., Wenderoth D, E, et al. (2004), Reduction in diversity of the colonic mucosa associated bacterial microflora in pients with active inflammatory bowel disease. Gut, 53(5), 685 -693. Patel E, K, Maloney N, S. et al (2010). Virus-plus- isceptibility gene interaction determines Crohn's disease gene Atg16L1 phenotypes in intestine. Cell, 141(7), 1135-1145.