This is an automatically translated article.
When something goes wrong with your blood, it can affect your overall health. That's why it's important for you to know about some of the common blood cell disorders that can affect you. The article will tell you more about the symptoms, types and causes of blood cell disorders.People can be affected by many different types of blood conditions and blood cancers. Common blood disorders include anemia, bleeding disorders such as hemophilia, blood clots, and blood cancers such as leukemia, lymphoma, and myeloma. Talking to your doctor is the first step to take if you believe you may have a blood disease. If you are diagnosed with a blood disorder, your doctor may refer you to a hematologist.
1. What is a blood cell disorder?
A blood cell disorder is a condition in which there are problems with red blood cells, white blood cells, or smaller circulating cells called platelets and are important for blood clot formation. All three types of cells form in the bone marrow and are the soft tissue inside your bones. Red blood cells carry oxygen to your body's organs and tissues. White blood cells help your body fight infections. Platelets help the blood to clot. A blood cell disorder is impaired formation and function of one or more of these types of blood cells.A blood disorder is any condition that affects one or more parts of the blood, often affecting the blood's ability to work properly.
Many blood disorders get their name by the composition of the blood they affect.
The following categories describe blood disorders that cause a decrease in blood components or affect their function:
Anemia - if the disorder involves red blood cells Leukopenia - if the disorder disorders affecting the white blood cells Thrombocytopenia - if the disorder involves platelets Types of blood disorders that increase the components of the blood:
Erythremia - if the disorder involves red blood cells Leukocytosis - if the disorder affects white blood cells Thrombocytosis - if the disorder involves platelets
2. Symptoms of Blood Cell Disorders
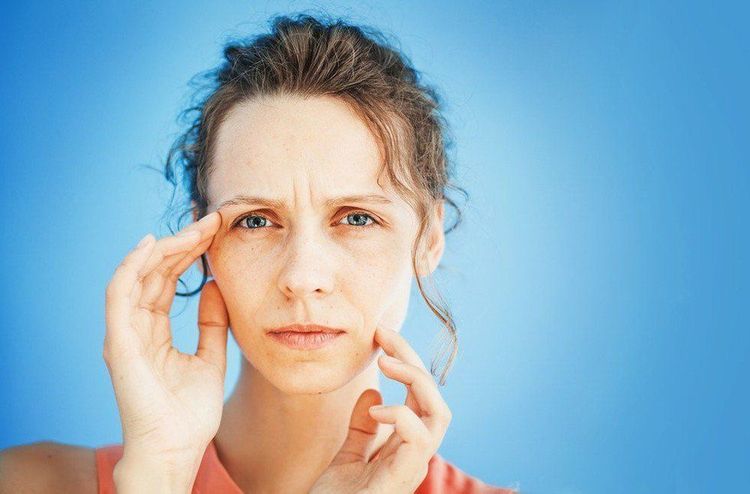
Symptoms will vary depending on the type of blood cell disorder. Common symptoms of a red blood cell disorder include:Fatigue Loss of breath Difficulty concentrating due to lack of oxygen in the brain Muscle weakness A rapid heartbeat Common symptoms of a white blood cell disorder include:
Chronic infections Fatigue Unexplained weight loss Irritability or general feeling of being unwell Common symptoms of a platelet disorder include:
Cuts or sores that won't heal or heal slowly Blood doesn't clot after an injury or cuts Easy bruising Unexplained nosebleeds or bleeding gums

Mệt mỏi là triệu chứng thường gặp của rối loạn tế bào máu
3. Types of blood cell disorders and causes
3.1 Red blood cell disorders Red blood cell disorders affect the body's red blood cells. These are the cells in your blood that carry oxygen from your lungs to the rest of your body. There are many types of this disorder, which can affect both children and adults.Anemia
Anemia is a type of red blood cell disorder. A lack of the mineral iron in your blood will often cause this disorder. Your body needs iron to produce the protein hemoglobin and to help red blood cells (RBCs) carry oxygen from your lungs to the rest of your body. There are many types of anemia.
Iron deficiency anemia: Iron deficiency anemia occurs when your body does not have enough iron. You may feel tired and short of breath because your red blood cells don't carry enough oxygen to your lungs. Iron supplements usually cure this type of anemia. Pernicious anemia: Pernicious anemia is an autoimmune condition in which your body cannot absorb adequate amounts of vitamin B-12. This leads to a low red blood cell count. It's called "pernicious," which means dangerous, because it was previously untreatable and often fatal. Currently, B-12 shots usually cure this type of anemia. Aplastic Anemia: Aplastic anemia is a rare but also serious condition in which your bone marrow stops making enough new blood cells. It can happen suddenly or gradually, and at any age. It can make you feel tired and unable to fight infections or bleed uncontrollably. Autoimmune hemolytic anemia (AHA): Autoimmune hemolytic anemia (AHA) causes your immune system to destroy red blood cells faster than your body can replace them. This results in you having too few RBCs. Sickle cell anemia: Sickle cell anemia (SCA) is a type of anemia that gets its name from the abnormal sickle-shaped shape of the affected red blood cells. Due to a genetic mutation, the red blood cells of people with sickle cell anemia contain abnormal hemoglobin molecules, which makes them stiff and curved. Sickle red blood cells can't carry as much oxygen to your tissues as normal red blood cells can. They can also get stuck in your blood vessels, impeding blood flow to your organs. Anemia during pregnancy : When the need for red blood cells is more than normal Thalassemia
Thalassemia is a group of inherited blood disorders. These disorders are caused by genetic mutations that prevent the normal production of hemoglobin. When red blood cells don't have enough hemoglobin, oxygen doesn't reach all parts of the body. The organs then do not function properly. These disorders can lead to:
Bone defects Enlarged spleen Heart problems Growth and development retardation in children Polycythemia vera
Polycythemia vera is a blood cancer caused by a genetic mutation. If you have polycythemia vera, your bone marrow makes too many red blood cells. This makes your blood thicker and flows more slowly, putting you at risk for blood clots that can cause heart attacks or strokes. There is no known cure. Treatment is with a veinectomy or removing blood from your veins and using medicine.
Malaria
Mosquito bites transmit the parasite into a person's bloodstream, where it infects red blood cells. Periodically, red blood cells burst, causing fever, chills, and organ damage. This blood infection is most common in parts of Africa but can also be found in other tropical and subtropical areas of the world; Those traveling to the affected areas should take precautions.
Thiếu máu là một loại rối loạn tế bào máu
The main types are:
Neutrophils, kill bacteria and viruses Lymphocytes, kill viruses, modulate the immune system Monocytes or macrophages that eat bacteria, viruses and fungi dead or disabled Basophils and eosinophils help your body respond to allergic reactions and help kill off parasites Some white blood cell disorders affect all different types of white blood cells in the blood, while other disorders involve only one or two specific types. Of the five types of white blood cells, neutrophils and lymphocytes are the most affected.
Most leukemic disorders are either cancerous or proliferative disorders.
Proliferative disorder associated with a rapid increase in the number of circulating white blood cells in the blood. This is mostly caused by an infection, although sometimes, bone marrow cancer can be the cause.
However, leukopenia is caused by a decrease in the number of circulating white blood cells. Leukopenia is often caused by:
Illness Infections Exposure to toxins Certain medications, such as corticosteroids or chemotherapy drugs Gene mutations Blood disorders that affect white blood cells include :
Lymphoma
A type of blood cancer that develops in the lymphatic system. In lymphoma, a white blood cell becomes malignant, multiplies, and spreads abnormally. Hodgkin's Lymphoma and Non-Hodgkin's Lymphoma are the two main groups of lymphoma. Treatment with chemotherapy and/or radiation therapy can often prolong survival with lymphoma, and sometimes cure the disease.
According to the American Cancer Society, non-Hodgkin lymphoma is one of the most common cancers in the United States, accounting for 4% of all cancers. An estimated 74,680 diagnoses will take place in the US in 2018. 70 percent of people diagnosed with non-Hodgkin lymphoma live at least 5 years after being diagnosed.
Hodgkin lymphoma will be much rarer than non-Hodgkin lymphoma. Again, according to the American Cancer Society, about 8,500 people in the United States had the disease in 2018. Of those diagnosed with Hodgkin lymphoma, 86% will live at least 5.
Leukemia
Leukemia involves the accumulation of abnormal white blood cells in the bone marrow, which interferes with its ability to produce red blood cells and platelets. Leukemia can be acute and develop rapidly, or chronic and develop gradually over time.
Chemotherapy and/or a stem cell transplant (bone marrow transplant) can be used to treat leukemia and possibly cure the disease.
The Leukemia & Lymphoma Association estimates that 60,300 people will be diagnosed with leukemia in 2018. Between 2007 and 2017, an estimated 63.7% of Americans diagnosed with leukemia live at least 5 after being diagnosed.
Myeloma
Myeloma involves the accumulation of plasma cells in the bone marrow, which interferes with the growth and function of other blood cells. The most common type of myeloma is multiple myeloma, a blood cancer in which a white blood cell called a plasma cell becomes malignant. Plasma cells multiply and release harmful substances, which eventually damage organs. Multiple myeloma has no cure, but stem cell transplants and/or chemotherapy can allow many people to live for many years with the condition.
According to the National Cancer Institute, from 2008-2014, about 50.7% of people had myeloma at least 5 years after being diagnosed. In general, myeloma is quite rare. In 2018, myeloma accounted for only 1.8% of all newly diagnosed cancer cases.
Myelodysplastic syndromes (MDS)
A family of blood cancers that affect the bone marrow. Your body makes too many immature cells, called blasts. The blasts multiply and squeeze the mature and healthy cells. The myelodysplastic syndrome usually progresses very slowly, but can suddenly turn into severe leukemia. Treatments may include blood transfusions, chemotherapy, and stem cell transplants.
Bệnh bạch cầu có liên quan tới rối loạn tế bào máu
Not enough platelets. Having too few platelets is dangerous because even a minor injury can cause serious blood loss. Too many platelets. If you have too many platelets in your blood, a blood clot can form and block a major artery, causing a stroke or heart attack. Platelets do not clot correctly. Sometimes, deformed platelets can't stick to other blood cells or the walls of your blood vessels, and so can't clot normally. This also has the potential to lead to dangerous blood loss. Platelet disorders are mostly genetic, which means they are inherited. Some of these disorders include:
Hemophilia
Hemophilia is an inherited condition caused by a lack or defect of clotting factors present in a person's blood. People with hemophilia will bleed longer or more heavily, both externally and internally, than people without the condition.
Hemophilia is probably the best known blood clotting disorder. It occurs almost always in men. The most serious complication of hemophilia is protracted and profuse bleeding. This bleeding can be inside or outside your body. Bleeding can start for no apparent reason. Treatment is with a hormone called desmopressin for mild type A, which can promote a reduced release of more clotting factors and blood and plasma transfusions for types B and C.
Hemophilia is often passed on from fathers. mothers to their children, but the National Hemophilia Foundation estimates that about a third of cases develop spontaneously. Hemophilia is one of the better known blood conditions, but it's still fairly rare, developing in about 1 in 5,000 live births.
Von Willebrand disease
Von Willebrand disease is the most common inherited bleeding disorder. It is caused by a deficiency in a protein that helps blood clot, called von Willebrand factor (VWF).
This disease occurs when the body lacks von Willebrand factor (VWF), a substance that allows platelets to stick together and form blood clots. Most von Willebrand cases are relatively mild, and people may only need treatment if they are injured or undergo surgery.
While many platelet disorders are related to a decrease in the number of platelets present in the blood or their function, a number of conditions can cause an excess of platelets.
Primary thrombocythemia
Primary thrombocythemia is a rare disorder that can lead to increased blood clotting. This puts you at a higher risk of having a stroke or heart attack. The disorder occurs when your bone marrow produces too many platelets, for unknown reasons; the platelets don't work properly, leading to excessive clotting, bleeding, or both.
Acquired platelet dysfunction
Certain medications and medical conditions can also affect how platelets work. Be sure to coordinate all of your medications with your doctor, even over-the-counter medications that you choose yourself. The Canadian Hemophilia Association (CHA) warns that the following common medications can affect platelets, especially if taken long-term.
Aspirin Non-steroidal anti-inflammatory drugs (NSAIDs) Certain antibiotics Heart drugs Blood thinners Antidepressants Anesthetics Antihistamines 3.4 Plasma cell disorders There are many disorders that affect blood cells plasma, the type of white blood cell in your body that makes antibodies. These cells are important to your body's ability to prevent infection and disease.
Plasma cell myeloma
Plasma cell myeloma is a rare blood cancer that develops in the plasma cells in the bone marrow. Malignant plasma cells accumulate in bone marrow tumors and form plasmacytomas, often concentrated in bones such as the spine, hips, or ribs. Abnormal plasma cells produce abnormal antibodies also known as monoclonal (M) proteins. These proteins have built up in the bone marrow, crowding out healthy proteins. This can lead to thick blood and kidney damage. The cause of plasma cell myeloma is not really known.
Hypercoagulable state (hypercoagulable state): Tends to cause blood to clot too easily; most people affected have only a slight tendency to excess blood clotting and may never be diagnosed. Some people develop repeated episodes of blood clots throughout their lives, and they have to take blood thinners every day.
Deep vein thrombosis : A blood clot in a deep vein, usually in the leg; Deep vein thrombosis can dislodge and travel through the heart to the lungs, causing a pulmonary embolism.
Disseminated intravascular coagulation (DIC): A condition that causes microscopic blood clots and areas of bleeding throughout the body simultaneously; Severe infections, surgery, or complications of pregnancy are conditions that lead to DIC.

Có thể điều trị rối loạn tế bào máu bằng thuốc
4. Treatment Options for Blood Cell Disorders
Your treatment plan depends on the cause, your age, and your overall health. Your doctor may use a combination of treatments to help correct your blood cell disorder.Medications Some pharmacotherapy options include drugs like Nplate (romiplostim) to stimulate the bone marrow to produce more platelets in a platelet disorder. For white blood cell disorders, antibiotics can help fight the infection. Dietary supplements such as iron and vitamins B-9 or B-12 can help treat deficiency anemia. Vitamin B-9 is known as folate and vitamin B-12 is also known as cobalamin.
Surgery A bone marrow transplant can repair or replace damaged marrow. They involve transferring stem cells, usually from a donor, into your body to help your bone marrow start producing normal blood cells. A blood transfusion is another option to help you replace lost or damaged blood cells. During a blood transfusion, you receive healthy blood from a donor.
Both processes require specific criteria for success. Bone marrow donors should match or be as close as possible to your genetic profile. A blood transfusion requires a donor with a compatible blood type.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: healthline.com, webmd.com, medicalnewstoday.com